Резюме
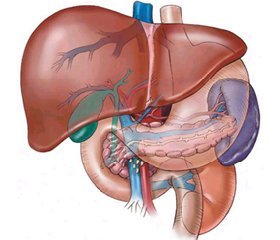
Мета роботи — оцінити ефективність застосування гепатопротекторів у комплексному лікуванні підлітків з неалкогольною жировою хворобою печінки та дисфункціональними біліарними розладами на тлі ожиріння. Матеріали та методи. Обстежено 80 підлітків 10–18 років з ожирінням та наявністю інсулінорезистентності. Усім проведено ультразвукове дослідження гепатобіліарної системи та біохімічне дослідження. У терапії ожиріння було застосовано метформін. За результатами обстеження хворих поділено на дві групи: 1-ша група — хворі з клінічними та ультразвуковими ознаками дисфункціональних розладів біліарного тракту (ДРБТ), яким призначались препарати екстракту артишоку; 2-га група — хворі з клінічними та ультразвуковими ознаками ДРБТ і біліарного сладжу, яким призначались препарати урсодеоксихолевої кислоти (УДХК). Контрольне обстеження проводилось після лікування та через 6 місяців. Результати. Підлітки з ожирінням скаржилися на підвищення апетиту, біль у животі та диспептичні розлади; у них визначалась болючість у правому підребер’ї, виявлено ознаки атерогенної дисліпідемії, а в третини хворих мали місце ознаки стеатогепатозу за даними ультразвукового дослідження. Призначення препаратів екстракту артишоку сприяло більш вираженому покращенню скорочувальної функції жовчного міхура та зменшенню ознак стеатогепатозу, ніж у групі порівняння. Лікування із застосуванням УДХК призвело до більш вираженого зменшення гіпотонії жовчного міхура та проявів стеатозу, гомогенізації жовчі, ніж у групі порівняння. Висновки. У підлітків з ожирінням та гіпотонією жовчного міхура обґрунтованим є призначення екстракту артишоку протягом 1,5–2 місяців. За ознак ДРБТ та біліарного сладжу доцільним є призначення препаратів УДХК протягом 2–3 місяців. Позитивний ефект від терапії через 6 місяців спостерігається лише у хворих, які були мотивовані щодо зміни способу життя.
Цель работы — оценить эффективность применения гепатопротекторов в комплексном лечении подростков с неалкогольной жировой болезнью печени и дисфункциональными билиарными расстройствами на фоне ожирения. Материалы и методы. Обследовано 80 подростков в возрасте 10–18 лет с ожирением и наличием инсулинорезистентности. Всем были проведены ультразвуковое исследование гепатобилиарной системы и биохимическое исследование. В терапии ожирения применяли метформин. По результатам обследования больные были разделены на две группы: 1-я группа — больные с клиническим и ультразвуковыми признаками дисфункциональных расстройств билиарного тракта (ДРБТ), которым назначались препараты экстракта артишока; 2-я группа — больные с клиническим и ультразвуковыми признаками ДРБТ и билиарного сладжа, которым назначались препараты урсодеоксихолевой кислоты (УДХК). Контрольное обследование проводилось после лечения и через 6 месяцев. Результаты. Подростки с ожирением жаловались на повышение аппетита, боль в животе и диспептические расстройства; у них определялась болезненность в правом подреберье, выявлены признаки атерогенной дислипидемии, а у трети больных имели место признаки стеатогепатоза по данным ультразвукового исследования. Назначение препаратов экстракта артишока способствовало более выраженному улучшению сократительной функции желчного пузыря и уменьшению признаков стеатогепатоза, чем в группе сравнения. Лечение с применением УДХК привело к более выраженному уменьшению гипотонии желчного пузыря и проявлений стеатоза, гомогенизации желчи, чем в группе сравнения. Выводы. У подростков с ожирением и гипотонией желчного пузыря обоснованным является назначение экстракта артишока в течение 1,5–2 месяцев. При наличии признаков ДРБТ и билиарного сладжа целесообразным является назначение препаратов УДХК в течение 2–3 месяцев. Положительный эффект терапии через 6 месяцев наблюдается лишь у больных, которые были мотивированы к изменению образа жизни.
Background. The purpose of the study is to evaluate the efficacy of hepatoprotectors in comprehensive treatment of adolescents with obesity, non-alcoholic fatty liver disease and dysfunctional disorders of the biliary tract (DDBT). Materials and methods. The study involved 80 adolescents with obesity and insulin resistance aged 10 to 18 years. Biochemical research and ultrasound investigation of the hepatobiliary system were conducted in all the patients. The metformin was used for all the patients in the treatment of obesity. According to the results of examination, all patients were divided into two groups: 1st group — patients with clinical and ultrasound signs of DDBT, who received artichoke extract preparations; 2nd group — patients with clinical and ultrasound signs of DDBT and biliary sludge, in whom ursodeoxycholic acid (UDCA) preparations were used. Control examinations were conducted after treatment and after the sixth month. Results. Adolescents with obesity complained of increased appetite, abdominal pain and dyspepsia. Pain in the right upper quadrant and signs of atherogenic dyslipidemia were determined in these patients. According to the ultrasound investigation, signs of steatohepatosis were found in one-third of patients. Improvement of contractile function of the gallbladder and decrease of steatohepatosis symptoms were more significant in those patients received artichoke extract preparations than in the comparison group. Homogenization of the bile, decrease in the signs of steatosis and hypotonia of the gallbladder were more significant in patients, who received UDCA preparations, than in the comparison group. Conclusions. The prescription of the artichoke extract preparations for the period of 1.5–2 months is reasonable for adolescents with obesity and hypotonia of the gallbladder. The administration of the UDCA preparations for the period of 2–3 months is reasonable in case of clinical signs of DDBT and biliary sludge presence. The positive effect of treatment after 6 months was observed only in patients, who were motivated to change their lifestyle.
Introduction
Obesity among children and adolescents is one of the most pressing problems of modern medicine. In almost all regions of the world the number of obese children and adolescents is steadily increasing and doubling every three decades. Obesity which began in childhood continues to progress in 60 % of the adult population and leads to serious complications, which are called “metabolic syndrome” [1, 2]. Obesity that started in childhood or adolescence and continues into the adult period has a more severe course. It is accompanied by a pronounced increase in the weight and frequency of concomitant dise-
ases than obesity which debuted in adulthood. The high frequency of disturbances of carbohydrate and lipid metabolism, arterial hypertension, dysfunction of the hepatobiliary system associated with obesity highlights the relevance of research problems of metabolic syndrome in this age group. These violations are manifestations of the complicated course of different degrees of obesity [3–6].
According to the results of epidemiological stu–dies non-alcoholic fatty liver disease (NAFLD) is a significant worldwide health problem with an estimated prevalence of 20–40 %. The probability of development of NAFLD increases significantly with increasing body mass index (BMI). NAFLD is regarded as hepatic manifestation of metabolic syndrome together with the most frequent manifestations such as insulin resistance, visceral obesity, dyslipidemia, diabetes mellitus type 2, arterial hypertension. Today there are no standards of treatment NAFLD based on the evidence base, therefore the main goal of therapy is to improve the biochemical indicators of inflammation, cytolysis, fibrogenesis. Anyway therapy should be started with lifestyle changes, change in diet, increase in physical activity. The most controversial issue is drug therapy of NAFLD [7–11].
The purpose of the study: to evaluate the effectiveness of differential use of hepatoprotectors in complex treatment of adolescents with obesity and pathology of the hepatobiliary system.
Materials and methods
80 adolescents with obesity aged from 10 to 18 years were examined at the Department of endocrinology of SI “Institute of Children and Adolescents Health Care of the NAMS of Ukraine”. The set of standard and special clinical and laboratory testing was conducted for them.
Ultrasound examination was performed according to the standard technique to evaluate structure-functional state of the liver. The presence of insulin resistance (IR) was determined by the HOMA index. Biochemical indicators of the protein (AST, ALT, ALP, GGTP, albumin, fibrinogen, prothrombin index), pigment (total bilirubin and its fractions) and lipid metabolism (triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDLc), low-density lipoprotein cholesterol (LDLc) and very low-density lipoprotein cholesterol (VLDLc), atherogenic coefficient (AC)) were determined according to the standard technique. Statistical analysis of the results was performed by methods of ma-thematical statistics for medical and biological researches with the help of software packages “Еxcell for Windows” and “Statistica 11.0 for Windows” (StatSoft Inc).
Results
We examined 80 obese patients with IR, 45 of them were boys — 56 % and 35 of them were girls — 44 %. The metformin was used orally for all the patients in the treatment of obesity in dose 500–850 mg (adjusted to patient’s age) 2 times a day for 3 months. Based on the results of clinical, laboratory instrumental methods of research all the patients were divided into two groups: 1st group (50 patients (63 %)) — patients with clinical and ultrasound signs of dysfunctional disorders of the biliary tract (DDBT), 2nd group (30 patients (37 %)) — patients with clinical and ultrasound signs of the DDBT and biliary sludge.
Clinically, such complaints from the side of digestive system were determined in patients with obesity: painfulness in the epigastrium in 46 — 57.5 ± 4.6 %, painfulness in the right upper quadrant in 52 — 64.5 ± 4.5 %, painfulness in the pyloroduodenal zone in 50 — 62.7 ± 4.6 %, painfulness in the left upper quadrant in 24 — 30.0 ± ± 4.3 %; painfulness associated with food intake in 52 — 65.4 ± 4.2 %, increased appetite in 63 — 78.8 ± 4.0 %, heartburn in the 50 — 63.6 ± 4.5 %, nausea in 43 — 53.8 ± 4.7 %, burp in 38 — 47.3 ± 4.7 %, constipation in 23 — 28.8 ± 4.2 %, diarrhea in 15 — 18.8 ± 3.6 %, vomiting in 9 — 11.3 ± 3.1 %. Thus, most patients with obesity complained about abdominal pain, increased appetite and motility disturbances of the upper gastrointestinal tract (heartburn, nausea, burp).
It was identified during the palpation that 74 patients had painfulness at the point of the gallbladder projection 92.5 ± 4.2 % and 58 patients had painfulness into the right upper quadrant 72.5 ± 4.2 %. Painfulness in the epigastric region was detected in more than half of the patients — 44 (55.0 ± 4.5 %) and the enlargement of the liver was detected in 41 (51.3 ± 4.7 %) during the palpation.
In the study of the liver functions was determined that mean levels of albumin, fibrinogen, prothrombin index, total bilirubin and liver enzymes were in the normal range. The findings suggest that adolescents with obesity probably don’t have severe violations of the functional state of the liver. Individual analysis of lipid profile parameters in children and adolescents with obesity showed that the pathological changes of lipid level were detected in 65.5 ± 5.1 % of patients, including 13.8 ± ± 2.1 % — increase of TC, 26.3 ± 4.7 % — decrease of HDLc, 28.8 ± 3.1 % — increase of TG, 31.3 ± 5.0 % — increase of VLDLc and AC. Thus, all adolescents with obesity showed signs of moderate atherogenic dyslipide-mia, which is characterized by increased levels of TG, VLDLc and tendency to reduced level of HDLc.
Ultrasound examination was performed to evaluate structure — functional state of the liver. However, diagnosis of early forms of NAFLD using the method of ultrasound study in children and adolescents causes some difficulties since clear criteria are not defined. The enlargement of the liver in 37.5 ± 4.0 % of patients with obesity was detected. The decrease in echogenicity of the liver was determined in 25.0 ± 4.6 % of patients, and its increase was determined only in the 10.0 ± 3.1 % of patients that testified about the adverse dynamics of pathological changes in the liver and the possible deve–lopment of steatohepatosis. Sealing of the walls of blood vessels were found in one third of adolescents with obesity 36.3 ± 5.2 %.
The enlargement of the gallbladder was found almost in all patients 98.8 ± 1.6 % and this was accompanied by the seal of its walls in 90.0 ± 2.5 %, by the presence of clumps of bile in 72.5 ± 3.9 %, by biliary sludge and parietal precipitate in 23.8 ± 4.4 % of patients. Hypotonic-hypokinetic type of dysfunction prevailed among dyskinetic disturbances of the gallbladder in adolescents with obesity 73.8 ± 3.9 %, hypotonic-hyperkinetic type of dysfunction was detected in 26.3 ± 4.0 % of the patients. Thus, clear signs of steatohepatosis according to the ultrasound examination were detected almost in one-third of adolescents with obesity.
Results of the clinical, laboratory instrumental stu–dies showed the presence of signs of violation of a condition of hepatobiliary system in adolescents with obesity. This was the justification for the prescription of different complexes of therapy for the correction of dyslipidemia, reduction of IR and disturbances of hepatobiliary system. Control examinations were conducted after treatment and after six month of starting treatment.
30 patients in 1st group (main subgroup) received preparations of artichoke extract in the combined therapy, and 20 patients (comparison subgroup) received only metformin as a basic treatment. The treatment lasted for 1,5–2 months. The treatment led to the improvement of well being in 28.7 % of the patients in the main subgroup and in 24.5 % of the patients in the comparison subgroup (p > 0.05); increased appetite and complaints about increased body weight were remained in 66.3 % of the patients in the main subgroup, and in 71.2 % of the patients in the comparison subgroup (p > 0.05). Abdominal pain was decreased in 33.3 % of the patients in the main subgroup and in 60.6 % of the patients in the comparison subgroup (p < 0.01), signs of dyspeptic syndrome were decreased in 65.8 % of the patients in the main subgroup and in 37.3 % of the patients in the comparison subgroup (p < 0.05) after treatment. An objective study showed that decrease of weight or tendency to its decrease was observed in 61.2 % of the patients in the main subgroup after treatment, and only in 38.5 % of the patients in the comparison subgroup (р < 0.05). Control ultrasound examination showed that size of the liver decreased in 55.7 % of the patients in the main subgroup and in 30.8 % of the patients in the comparison subgroup (р < 0.05), normalization of the echogenicity of the hepatic parenchyma was detected in 33.3 % of the patients in the main subgroup and in 20.5 % of the adolescents in the comparison subgroup (р < 0.05). Contractile function of the gallbladder was improved in 27.7 % of the patients in the main subgroup and was unchanged in the comparison subgroup (p < 0.05). Analysis of the result of lipid profile parameters of group 2 showed a tendency to positive antiatherogenic changes of the average indices of TG, HDLc, LDLc and VLDLc. Individual analysis of lipid profile parameters showed that the reduction in atherogenic lipoprotein fractions and TG (even within normal values) occurred in 60.4 % of the patients in the main subgroup and in 40.5 % of the patients in the comparison subgroup (p > 0.05).
Control tests of patients with obesity after 6 months of treatment in this group showed decreased appetite and weight loss in 30.5 % of the patients of the main subgroup and in 25.7 % of the patients in the comparison subgroup (р > 0.05). Complaints about abdominal pain were left in 44.3 % of the patients in the main group and in 74.8 % of the patients in the comparison subgroup (p < 0.05). Dyspepsia remained in 33.3 % of the patients in the main group and in the majority of patients in the comparison subgroup (83.5 % (p < 0.05)). Normalization of lipid profile was diagnosed in 50.8 % of the patients in the main subgroup, and in 40.5 % of the patients in the comparison subgroup (p > 0.05). Improvement of function of biliary system was detected in 35.7 % of the patients in the main subgroup, signs of hypotension of gallbladder remained in all the patients in the comparison subgroup (p < 0.01). Control ultrasound examination showed that size of the liver decreased in 70.3 % of the patients in the main subgroup and in 40.2 % of the patients in the comparison subgroup (р < 0.05), normalization of the echogenicity of the hepatic parenchyma was detected in 63.8 % of the patients in the main subgroup and in 27.7 % of the adolescents in the comparison subgroup (р < 0.05). Positive results of treatment were determined in those adolescents with obesity who adhered to recommendations on diet and physical activity.
12 patients in 2nd group (main subgroup) received preparations of ursodeoxycholic acid (UDCA) in the age dosages (calculated per kg of body weight) in the combined therapy, and 18 patients (subgroup comparisons) received only metformin in the basic treatment. The treatment lasted for 2–3 months. Improvement of well being was showed in 32.5 % of the patients in the main subgroup after treatment with UDCA and in 21.5 % of the patients in the comparison subgroup on the background of basic therapy (p > 0.05). Complaints about abdominal pain were left in 43.8 % of the patients in the main subgroup, in 60.2 % of the patients in the comparison subgroup (p < 0.05); signs of dyspeptic syndrome disappeared or significantly decreased in 70.2 % of the patients in the main subgroup and in 30.3 % of the patients in the comparison subgroup (p < 0.05). An objective study showed that decrease of weight or tendency to its decrease was observed in 60.2 % of the patients in the main subgroup after treatment, and only in 30.3 % of the patients in the comparison subgroup (р < 0.05). Control ultrasound examination showed that size of the liver decreased in 75.3 % of the patients in the main subgroup and in 33.3 % of the patients in the comparison subgroup (р < 0.05), normalization of the echogenicity of the hepatic parenchyma was detected in 75.5 % of the patients in the main subgroup and in 20.8 % of the adolescents in the comparison subgroup (р < 0.05). Contractile function of the gallbladder was improved in 40.5 % of the patients in the main subgroup and was unchanged in the comparison subgroup (p < 0.05). Echostructure of bile was homogeneous, parietal precipitate was not detected in 60.2 % of the patients in the main group. Echostructure of bile was unchanged in the comparison subgroup. The results of parameters of lipid profile in patients of group 3 testified to the positive impact of both schemes of treatment — basic therapy with metformin, and treatment with metformin and UDCA. Both variants of treatment resulted in improvement of lipid profile: level of atherogenic fractions of lipoproteins and TG decreased in half of the patients in the main subgroup and in the comparison subgroup.
Control tests of the patients with obesity showed reduction of appetite and weight loss in 35 % of the patients in the main subgroup and in 20 % of the patients in the comparison subgroup after 6 months of treatment in this group (р < 0.05). Complaints about abdominal pain were left in 20.5 % of the patients in the main group and in 56.3 % of the patients in the comparison subgroup (p < 0.05). Dyspeptic symptoms were absent in the main subgroup and presented almost in half of the patients in the comparison subgroup (p < 0.05). Normalization of lipid profile was diagnosed in 60.6 % of the patients in the main subgroup, and in 32.3 % of the patients in the comparison subgroup (p < 0.05). Control ultrasound examination showed the positive changes in 40.1 % of the patients in the main subgroup (who was motivated on lifestyle modification) after 6 months. The state of the biliary system was unchanged in the patients in the comparison subgroup at the same time. Normalization of the size of the liver and the echogenicity of the hepatic parenchyma was detected in 83.3 % of the patients in the main subgroup and in 40.1 % of the patients in the comparison subgroup (р < 0.05) (table 1).
%201/18-1.jpg)
Conclusions
Pathology of the hepatobiliary system was diagnosed almost in all adolescents with obesity. Signs of DDBT in the form of gallbladder hypotonia in 98 % of the adolescents with obesity, bile clots in the gallbladder in 73 % of the patients, biliary sludge and parietal precipitate in 24 % of the patients, signs of the liver steatosis in 33 % of the patients were detected according to clinical, laboratory instrumental studies.
Basic treatment of adolescents with obesity with the presence of insulin resistance, includes metformin orally in dose 500–850 mg (adjusted to patient’s age) 2 times a day for 3 months. Use of metformin contributed to a reduction in appetite and in weight (or at least tendency to weight loss) in 20–30 % of the patients within 6 months of starting treatment regardless of complexes of treatment, also positively influenced the quality of the lipid spectrum of blood by reducing atherogenic phenomena.
1. The use of preparations of artichoke extract in the age dosage for 1,5–2 months in the combined treatment is justified in the case of presence clinical and ultrasound signs of DDBT in the form of gallbladder hypotonia in adolescents with obesity. It helps to improve function of biliary system that is proved by the decrease of signs of the gallbladder hypotonia in one third of the patients after 3 months of starting treatment and persists after 6 months. The appointment of preparations of artichoke extract on the background of metformin therapy resulted in more significant reduction of the signs of steatohepatosis both after 3 and after 6 months of starting treatment than in patients who received only metformin.
2. The appointment of the UDCA preparations in combined therapy for the period of 2–3 months is reaso–nable in case of clinical and ultrasound signs of the DDBT and biliary sludge in adolescents with obesity. This helps to improve contractile function of the gallbladder with homogenization of bile in the gallbladder. Also reduction of the liver size and normalization of its echogenicity in half of the patients after 3 months of starting treatment and stabilization of these parameters after 6 months of starting treatment were shown.
3. Analysis of the results of treatment after 6 months, regardless of the therapeutic complex, showed a positive effect only in those patients who were motivated to change their lifestyle, what primarily means to observe the diet and physical activity. This demonstrates the need for the creation and implementation of educational programs for the treatment of obesity and prevention of its complications.
Conflict of interests. Authors declare the absence of conflict of interests.
Список литературы
1. Висцеральное ожирение как предиктор атерогенеза у больных с неалкогольной жировой болезнью печени / Г.Д. Фадеенко, Т.А. Соломенцева, К.А. Сытник [и др.] // Сучасна гастроентерологія. — 2015. — № 2(82). — С. 22-27.
2. Красноперова О.И. Факторы, приводящие к развитию ожирения у детей и способствующие его трансформации в метаболический синдром / О.И. Красноперова, Е.Н. Смирнова, Н.Б. Мерзлова // Фундаментальные исследования. — 2012. — № 4. — C. 306-310.
3. Ягмур В.Б. Неалкогольна жирова хвороба печінки: сучасний погляд на патогенез, діагностику та лікування / В. Б. Ягмур // Гастроентерологія. — 2013. — № 3(49). — С. 138-147.
4. Cardiometabolic risks and severity of obesity in children and young adults / Skinner A., Perrin E., Moss L., Skelton J. // N. Engl. J. Med. — 2015. — Vol. 373, № 14. — Р. 1307-1317. doi: 10.1056/NEJMoa1502821.
5. Preventing obesity and eating disorders in adolescents / Golden N.H., Schneider M., Wood C. et al. // Pediatrics. — 2016. — Vol. 138, № 3. doi: 10.1542/peds.2016-1649.
6. Pediatric Obesity — Assessment, Treatment, and Prevention: An Endocrne Society Clinical Practice Guideline / Styne D.M., Arslanian S.A., Connor E.L. et al. // J. Clin. Endocrinol. Metab. — 2017. — Vol. 102, № 3. — P. 709-757. doi: 10.1210/jc.2016-2573.
7. Колесникова Е.В. Диагностика и лечение больных с неалкогольной жировой болезнью печени: практические рекомендации Американской ассоциации по изучению заболеваний печени, Американского колледжа гастроэнтерологии и Американской гастроэнтерологической ассоциации (2012) / Е.В. Колесникова // Сучасна гастроентерологія. — 2014. — № 3(77). — С. 89-104.
8. Зайченко О.Е. Терапевтические мишени при неалкогольной жировой болезни печени / О.Е. Зайченко // Сучасна гастроентерологія. — 2014. — № 1(75). — С. 130-138.
9. Радченко О.М. Неалкогольна жирова хвороба печінки: проблеми лікування / О.М. Радченко // Рациональная фармакотерапия. — 2012. — № 3(24). — С. 9-13.
10. Dietary Approaches to Stop Hypertension (DASH) dietary pattern is associated with reduced incidence of metabolic syndrome in children and adolescents / Asghari G., Yuzbashian E., Mirmiran P. et al. // J. Pediatr. — 2016. —Vol. 174. — P. 178-184. doi: 10.1016/j.jpeds.2016.03.077.
11. Kim D., Kim W.R. Nonobese Fatty Liver Disease / D. Kim, W.R. Kim // Clin. Gastroenterol. Hepatol. — 2017. — Vol. 15, № 4. — P. 474-485. doi: 10.1016/j.cgh.2016.08.028.

%201/18-1.jpg)