Международный эндокринологический журнал Том 18, №5, 2022
Вернуться к номеру
Оцінка 10-річного серцево-судинного ризику і 8-річного ризику цукрового діабету з використанням Фремінгемської шкали в осіб із предіабетом
Авторы: Neeta Kumari (1), Deepak Kumar Verma (2), B.K. Binawara (3)
(1) — Department of Physiology, S.M.M.H. Medical College, Saharanpur, C.C.S. University, Meerut, India
(2) — Department of Pharmacology, S.M.M.H. Medical College, Saharanpur, C.C.S. University, Meerut, India
(3) — Department of Physiology, S.P. Medical College, Rajasthan University of Health, Jaipur, India
Рубрики: Эндокринология
Разделы: Клинические исследования
Версия для печати
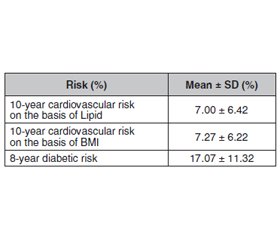
Актуальність. Предіабет — це стан, що характеризується порушенням глікемії натще або порушенням толерантності до глюкози. Предіабет сприяє підвищеному ризику виникнення серцево-судинних ускладнень. Різноманітні фактори ризику є причиною прогресування серцево-судинних захворювань і цукрового діабету (ЦД) 2-го типу в осіб із предіабетом. Мета дослідження: визначення 10-річного серцево-судинного ризику і 8-річного ризику ЦД за допомогою Фремінгемської шкали в осіб із предіабетом. Матеріали та методи. Перехресне дослідження було проведено на кафедрі фізіології Медичного коледжу та Університетської лікарні у співпраці з діабетичним дослідницьким центром. Особи з предіабетом були ідентифіковані серед родичів першого ступеня пацієнтів із ЦД 2-го типу, зареєстрованих у дослідницькому центрі діабету. Особи з предіабетом (порушенням рівня глікемії натще, ПГН) були ідентифіковані на основі рівня глюкози в крові натще від 100 до 125 мг/дл і глікованого гемоглобіну HbA1c від 5,7 до 6,4 % згідно з рекомендаціями Американської діабетичної асоціації. Послідовний відбір проб проводився доти, доки розмір вибірки не став відповідати критеріям дослідження. До дослідження були включені суб’єкти вікової групи 20–74 роки, які мали ПГН від 100–125 мг/дл, HbA1c від 5,7 до 6,4 % і дали інформовану письмову згоду. Програма Pre-structured Performa використовувалася для збору загальної інформації, соціально-демографічної інформації, базових характеристик, особистих звичок, біохімічного аналізу й параметрів крові. 10-річний ризик розвитку серцево-судинних захворювань і 8-річний ризик розвитку цукрового діабету оцінювали за допомогою Фремінгемської шкали. Результати. Вік, професія, індекс маси тіла, дієта, куріння, алкоголь, вісцеральне ожиріння та сімейний анамнез цукрового діабету були вірогідно пов’язані з поширеністю цукрового діабету 2-го типу й предіабету, тоді як стать і грамотність — ні. Висновки. У цьому дослідженні було виявлено, що похилий вік, професійні зміни, індекс маси тіла, куріння, ожиріння, недостатня фізична активність, підвищений артеріальний тиск і сімейний анамнез діабету були значною мірою пов’язані з майбутнім ризиком розвитку цукрового діабету 2-го типу і серцево-судинних захворювань серед пацієнтів із предіабетом.
Background. Prediabetes is a state characterized by impaired fasting glucose or impaired glucose tolerance. This implies that prediabetes bears an increased risk of cardiovascular complications. Various risk factors are the reason of the progression of cardiovascular diseases and type 2 diabetes mellitus (T2DM) in prediabetics if factors are not overt. Hence, the present study was undertaken to determine the future 10-year cardiovascular and 8-year diabetic risk by using Framingham heart scale in prediabetic subjects. Materials and methods. Present cross-sectional study was carried out at Department of Physiology, S.P. Medical College & Hospital in collaboration with Diabetic Research Centre P.B.M. Hospital Bikaner (Rajasthan). Prediabetic subjects were identified from first-degree relatives of T2DM patients, enrolled in Diabetic Research Centre P.B.M. Hospital Bikaner. Prediabetics (impaired fasting glucose) subjects were identified on the basis of fasting blood glucose of 100 to 125 mg/dl and HbA1c (5.7 to 6.4 %) as per American Diabetes Association 2011 guidelines. Consecutive sampling was conducted till sample size satisfied during the period of study. Subjects of age group 20–74 years who had fasting blood glucose of 100–125 mg/dl, HbA1c of 5.7 to 6.4 % and gave informed written consent were included in study. Pre-structured performa was used to collect general information, sociodemographic information, baseline physical characteristics, personal habits, biochemical analysis, and for blood parameters. Future 10-year cardiovascular and 8-year diabetic risk were assessed by using Framingham heart scale. Results. Age, occupation, body mass index, diet, smoking, alcohol, truncal obesity and family history of diabetes were significantly associated with the prevalence of T2DM/prediabetes whereas gender and literacy were not. Conclusions. In the present study, it was observed that advanced age, occupational changes, body mass index, substance abuse like smoking, central obesity, exercise, blood pressure and family history of diabetes were highly associated with future risk of T2DM and cardiovascular diseases among prediabetic subjects of first-degree relatives.
предіабет; серцево-судинні захворювання; цукровий діабет 2-го типу; фактори ризику; Фремінгемська шкала
prediabetes; Framingham scale; cardiovascular disease; diabetes; risk factors
Introduction
Materials and methods
Socioeconomic status
Family history of DM
Smoking and alcohol
Demographical division
Biochemical parameters
Results
/8.jpg)
/8_2.jpg)
Discussion
/9_2.jpg)
Conclusions
- American Diabetes Association Professional Practice Committee. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022. 45 (Suppl. 1). S17-S38. doi: 10.2337/dc22-S002.
- van Herpt T.T.W., Ligthart S,. Leening M.J.G., van Hoek M., Lieverse A.G., Ikram M.A., Sijbrands E.J.G. et al. Lifetime risk to progress from pre-diabetes to type 2 diabetes among women and men: comparison between American Diabetes Association and World Health Organization diagnostic criteria. BMJ Open Diabetes Res Care. 2020. 8(2). e001529. doi: 10.1136/bmjdrc-2020-001529.
- Nasykhova Y.A., Tonyan Z.N., Mikhailova A.A., Danilova M.M., Glotov A.S. Pharmacogenetics of Type 2 Diabetes-Progress and Prospects. Int. J. Mol. Sci. 2020. 21(18). 6842. doi: 10.3390/ijms21186842.
- Bhutta Z.A., Salam R.A., Gomber A., Lewis-Watts L., Narang T., Mbanya J.C., Alleyne G. A century past the discovery of insulin: global progress and challenges for type 1 diabetes among children and adolescents in low-income and middle-income countries. Lancet. 2021. 398(10313). 1837-1850. doi: 10.1016/S0140-6736(21)02247-9.
- Hu H., Wang J., Han X., Li Y., Miao X., Yuan J., Yang H., He M. Prediction of 5-year risk of diabetes mellitus in relatively low risk middle-aged and elderly adults. Acta Diabetol. 2020. 57(1). 63-70. doi: 10.1007/s00592-019-01375-w.
- Rodgers L.R., Hill A.V., Dennis J.M., Craig Z., May B., Hattersley A.T., McDonald T.J. et al. Choice of HbA1c threshold for identifying individuals at high risk of type 2 diabetes and implications for diabetes prevention programmes: a cohort study. BMC Med. 2021. 19(1). 184. doi: 10.1186/s12916-021-02054-w.
- Preis S.R., Pencina M.J., Mann D.M., D’Agostino R.B. Sr, Savage P.J., Fox C.S. Early-adulthood cardiovascular disease risk factor profiles among individuals with and without diabetes in the Framingham Heart Study. Diabetes Care. 2013. 36(6). 1590-6. doi: 10.2337/dc12-1121.
- Fox C.S. Cardiovascular disease risk factors, type 2 diabetes mellitus, and the Framingham Heart Study. Trends Cardiovasc. Med. 2010. 20(3). 90-5. doi: 10.1016/j.tcm.2010.08.001.
- Bitton A., Gaziano T.A. The Framingham Heart Study’s impact on global risk assessment. Prog. Cardiovasc. Dis. 2010. 53(1). 68-78. doi: 10.1016/j.pcad.2010.04.001.
- Mahmood S.S., Levy D., Vasan R.S., Wang T.J. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Lancet. 2014. 383(9921). 999-1008. doi: 10.1016/S0140-6736(13)61752-3.
- Ramachandran A., Snehalatha C., Vijay V., King H. Impact of poverty on the prevalence of diabetes and its complications in urban southern India. Diabet Med. 2002. 19(2). 130-5. doi: 10.1046/j.1464-5491.2002.00656.x.
- Das M., Pal S., Ghosh A. Family history of type 2 diabetes and prevalence of metabolic syndrome in adult Asian Indians. J. Cardiovasc. Dis. Res. 2012. 3(2). 104-8. doi: 10.4103/0975-3583.95362.
- Tripathy J.P., Thakur J.S., Jeet G., Chawla S., Jain S., Pal A. et al. Prevalence and risk factors of diabetes in a large community-based study in North India: results from a STEPS survey in Punjab, India. Diabetol. Metab. Syndr. 2017. 9. 8. doi: 10.1186/s13098-017-0207-3.
- Fryar C.D., Carroll M.D., Gu Q., Afful J., Ogden C.L. Anthropometric Reference Data for Children and Adults: United States, 2015–2018. Vital Health Stat. 3. 2021. 36. 1-44. PMID: 33541517.
- Sarkar D., Latif S.A., Uddin M.M., Aich J., Sutradhar S.R., Ferdousi S. et al. Studies on serum lipid profile in hypertensive patient. Mymensingh Med. J. 2007. 16(1). 70-6. doi: 10.3329/mmj.v16i1.252. PMID: 17344784.
- Nigam P.K. Serum Lipid Profile: Fasting or Non-fasting? Indian J. Clin. Biochem. 2011. 26(1). 96-7. doi: 10.1007/s12291-010-0095-x.
- D’Agostino R.B. Sr, Vasan R.S., Pencina M.J., Wolf P.A., Cobain M., Massaro J.M., Kannel W.B. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008. 117(6). 743-53. doi: 10.1161/CIRCULATIONAHA.107.699579.
- Wilson P.W., Meigs J.B., Sullivan L., Fox C.S., Nathan D.M., D’Agostino R.B. Sr. Prediction of incident diabetes mellitus in middle-aged adults: the Framingham Offspring Study. Arch. Intern. Med. 2007. 167(10). 1068-74. doi: 10.1001/archinte.167.10.1068.
- Chodick G., Elchalal U., Sella T., Heymann A.D., Porath A., Kokia E., Shalev V. The risk of overt diabetes mellitus among women with gestational diabetes: a population-based study. Diabet Med. 2010. 27(7). 779-85. doi: 10.1111/j.1464-5491.2010.02995.x.
- Beulens J., Rutters F., Rydén L., Schnell O., Mellbin L., Hart H.E., Vos R.C. Risk and management of pre-diabetes. Eur. J. Prev. Cardiol. 2019. 26 (Suppl. 2). 47-54. doi: 10.1177/2047487319880041. PMID: 31766914.
- Asha Shrivastava, Namit Garg, Rashmi Dave. HbA1c: Future Diabetic and Cardiovascular Risk in First Degree Relatives of Type 2 Diabetes Mellitus. IJBAP. 2013. 2(1). 79-82. DOI: 10.5281/zanodo.4483066.
- Bisht Inderamohan, Dhanda Saurabh, Chauhan Suman, Yadav Rajinder, Yadav Suman. Prevalence of prediabetes in apparently healthy population of Tehsil Kangra and adjoining areas. International Journal of Community Medicine and Public Health. 2018. 5. 4916. Doi: 10.18203/2394-6040.ijcmph20184596.
- Bhalerao Sanjay, Somannavar Manjunath, Vernekar Sunil, Rajashree R., Shivaprasad Goudar. Risk factors for type 2 diabetes mellitus in rural population of North Karnataka: A community-based cross-sectional study. International Journal of Pharma Medicine and Biological Sciences. 2014. 3(1). 1-14.
- Ramaswamy G., Chinnakali P., Selvaraju S., Nair D., Thekkur P., Selvaraj K. et al. High prevalence of prediabetes among the family members of individuals with diabetes. Findings from targeted screening program from south India. Diabetes Metab. Syndr. 2019. 13(1). 866-872. doi: 10.1016/j.dsx.2018.12.001.
- Maddatu J., Anderson-Baucum E., Evans-Molina C. Smoking and the risk of type 2 diabetes. Transl. Res. 2017 Jun. 184. 101-107. doi: 10.1016/j.trsl.2017.02.004.
- Campagna D., Alamo A., Di Pino A., Russo C., Calogero A.E., Purrello F., Polosa R. Smoking and diabetes: dangerous liaisons and confusing relationships. Diabetol. Metab. Syndr. 2019. 11. 85. doi: 10.1186/s13098-019-0482-2.
- Cai X., Chen Y., Yang W., Gao X., Han X., Ji L. The association of smoking and risk of diabetic retinopathy in patients with type 1 and type 2 diabetes: a meta-analysis. Endocrine. 2018. 62(2). 299-306. doi: 10.1007/s12020-018-1697-y.
- Yuan S., Xue H.L., Yu H.J., Huang Y., Tang B.W., Yang X.H. et al. Cigarette smoking as a risk factor for type 2 diabetes in women compared with men: a systematic review and meta-analysis of prospective cohort studies. J. Public Health (Oxf.). 2019. 41(2). e169-e176. doi: 10.1093/pubmed/fdy106. PMID: 29901755.

/9.jpg)