Introduction
Fibrillary glomerulonephritis (FGN) or fibrillary glomerulopathy (FGP) is a glomerulopathy that is classified into two groups of congophobic and congophilic fibrillary glomerulonephritis. Diagnosis of fibrillary glomerulonephritis is made by kidney biopsy. The commonest light microscopic finding is membranoproliferative glomerulonephritis. Mesangial proliferation, endocapillary proliferation and diffuse glomerulosclerosis are the other histologic patterns in light microscopy. Membranous nephropathy, cellular of fibrocellular crescents and interstitial fibrosis may be present in histologic presentation of disease. In immunofluorescence microscopy, all patients are stained with immunoglobulins, C3 and C1q, kappa and lambda chains. The texture of staining was smudged without linearity or granularity. Ultrastructural evaluation of kidney specimens is done by presence of fibrils as random orientation, width of < 30 nanometer (nm), no hollow cores in magnifications more than × 30000 and positive immunoglobulins by immunofluorescence (IF) staining [1]. Dna-j heat shock protein family B member 9 (DNAjB9) that, namely known as endoplasmic reticulum-localized DnaJ homologs 4 (ERdj4) or mdg-1, is a 223 amino acid member of the DNAJ family of proteins that act as co-chaperones for the heat shock protein 70 family members including binding immunoglobulin protein (BiP). The heat shock protein (HSP) 70 family members are thought as important chaperones in the endoplasmic reticulum (ER) and involve in protein folding, unfolding, translocation and degradation [2]. The J-domain of Dnaj has a histidine-proline-aspartic acid motif which stimulates hydrolysis of adenosine triphosphate (ATP) [3]. DnaJB9 was first discovered in 2002 and there is in ER organs such as liver, placenta and kidneys. There is no specific treatment for fibrillary glomerulonephritis and renal prognosis is poor. Patients achieve to end-stage kidney disease (ESKD) with mean average of 4 years after diagnosis. Kidney transplantation is an option for ESKD patients and recurrence can occur post renal transplant period.
Objectives
Research questions
Why DNAjB9 marker is diagnostic biomarker
DNAjB9 histochemical marker is abundantly detected in glomeruli of fibrillary glomerulopathy, in glomeruli of healthy persons and not in glomeruli of other glomerular diseases. This marker distinguishes congophilic fibrillary glomerulonephritis from amyloidosis in kidney biopsy specimens. Hence, it accounts as a 100% specific and sensitive survey in fibrillary glomerulopathy and can be used as quick and specific diagnostic method for this disease in the absence of ultrastructural evaluation.
What DNAjB9 biomarker does
DNAjB9 immunohistochemical biomarker is a member of molecular chaperone gene family that is analyzed using mass spectrometry or laser microdissection-assisted shotgun proteomics in glomeruli of kidney specimens in patients with fibrillary GP. As previously mentioned, DNAjB9 involves in BIP as a co-chaperone, assisting in protein folding and degradation of misfolded protein as unfolded protein response (UPR). In other words, DNAjB9 involves in recognition of misfolded protein and marks them for degradation. It may inhibit apoptotic effect of p53 on cells with stress and this function indicates that increased expression of DNAjB9 may be a marker for increased ER stress. DNAjB9 is found in low levels in ER in most of cell types such as cytoplasm of neurons, gastrointestinal (GI), gynecologic, pulmonary, breast epithelium and lymphocytes. In the normal kidney, DNAjB9 is detected in renal tubular epithelial cells, podocytes, mesangial and endothelial cells. Existing large amounts of DNAjB9 marker in extracellular deposition distinguishes it from other glomerular diseases and this finding is specific for this disease.
Materials and Methods
Eligibility Criteria
Type of Studies
The search identified 3045 full-text articles via electronic search in google scholar (2690), PubMed central (318) and other databases (37). Therefore total records of 3045 full-text articles were identified and five articles were deduplicated (3040). So total 3040 articles screened based on title and abstract. Then 66 full-text articles were eligible and 2974 articles were excluded due to not related subject. Therefore, 72 participants in 62 published articles included and 4 articles were discarded due to non-case reports. These 62 articles included 72 case reports that were examined 72 patients of kidney disturbation as decreased estimated glomerular filtration rate (eGFR) or elevated serum creatinine. These participants were enrolled for systematic review and meta-analysis.
Type of Participants
All patients with biopsy-proven fibrillary glomerulopathy were considered in this research.
Type of Outcomes
Primary end-points. Proportion of acute kidney injury (AKI), acute kidney disease (AKD), chronic kidney disease (CKD) and non-kidney disease (NKD), graft loss, proteinuria, relative risk (RR) and Odds ratio (OR) of kidney failure progression to kidney replacement therapy (KRT), death probability and effect of DNAjB9 marker on outcome of fibrillary glomerulopathy were considered as primary end-points.
Secondary end-points. Decreased estimated glomerular filtration rate, positive anti-nuclear antibodies (ANA), positive cryoglobulins, low complement levels, positive viral infection, low platelet counts and high hepatic enzyme levels are considered as secondary end-points.
Information Sources. The paper has written based on advanced searching via PubMed and Google Scholar databases to identify articles published since 1975 to January 2022.
Search methods for identification of studies
Electronic search
The mentioned search performed with search terms of fibrillary deposition And (Boolean) kidney impairement, also with term of fibrillary glomerulopathy in this research.
Searching other resources
The author reviewed references of all included articles and performed handsearching of related journals to identify the additional relevant studies.
Study selection
The search strategy was used to obtain titles and abstracts of articles in databases. Total 3045 titles and abstracts were identified via electronic search in PubMed and Google Scholar by author. Total records of 3045 articles were identified and eventually 3040 articles identified after deduplication. Therefore, 3040 articles screened in this research. Of these, 2974 articles were excluded due to non-related subject, review articles, others and 66 full-text articles were considered for eligibility. However studies and reviews that might include relevant data or information on studies were retained initially. Four articles were excluded and then 62 published articles were included for qualitative and quantitative synthesis. These 62 published articles were enrolled 72 patients with fibrillary glomerulonephritis with kidney specimens in current research.
Data collection and analysis
Data extraction and management
Data extraction was carried out by author and studies which reported in journals as non-English language were translated before assessment. Where more than one publication of a study existed, reports were grouped together and the publication with the most complete data was included.
Data items
All patients with clinical, laboratory and pathologic presentations of fibrillary GN, decreased eGFR and tissue biopsy-proven kidney specimens were considered in this research. Demographic and clinical features such as age, sex, different symptoms and physical signs were extracted from this study. Furthermore, biochemical variables of serum creatinine (SCr), eGFR, urine protein at initial presentation and following days, imaging, management and outcomes were collected.
Definition of kidney dysfunction
AKI, AKD and CKD, NKD can form a continuum whereby initial kidney injury can lead to persistent injury eventually leading to CKD. AKI is defined as an abrupt decrease in kidney function occurring over 7 days or less whereas CKD is defined by the persistent of kidney disease for a period of > 90 days. AKD is defined as acute or subacute damage and/or loss of kidney function for duration of seven and 90 days after exposure to an AKI initiating event. Recovery from AKI within 48 h of the initiating event typically heralds rapid reversal of AKI [16th workgroup of acute disease quality initiative (ADQI) consensus report in 2017]. Kidney disease: improving global outcomes (KDIGO) in August 2020 convened a consensus conference for kidney disease definition as functional and/or structural abnormalities of the kidney and classified kidney disease (KD) according to cause, severity of structural and functional abnormalities and duration of those abnormalities (KDIGO consensus conference 2020, published in July 2021). Based on this classification, KD can be classified to AKI, AKD, CKD and NKD. CKD is classified according to eGFR and kidney damage such as proteinuria (> 200 mg/day or protein to creatinine ratio > 200 mg/g creatinine) or albuminuria (urinary albumin excretion ≥ 30 mg/day or albumin to creatinine ratio ≥ 30 mg/g creatinine) using SCr. Kidney di–sease outcomes: quality initiative (KDOQI) guidelines 2009 classified CKD to stage 0 (no CKD) corresponded to eGFR ≥ 90 ml/min/1.73 m2 without proteinuria, Stage 1 to eGFR ≥ 90 mL/min/1.73 m2 with proteinuria, Stage 2 to eGFR ≥ 60–90 mL/min/1.73 m2, Stage 3 to eGFR ≥ 30–60 mL/min/1.73 m2, Stage 4 to eGFR ≥ 15–30 mL/min/1.73 m2 and Stage 5 to eGFR ≤ 15 mL/min/1.73 m2 or end-stage renal disease (ESRD) requiring the initiation of chronic dialysis therapy [4]. 2012 KDIGO CKD guidelines classified CKD to cause of disease, level of GFR (6 categories), and level of albuminuria (3 categories), collectively classified with mnemonic of CGA. Of course this key point must be said that term of nephrology-related conditions must be used instead of kidney diseases [5]. Estimated GFR is defined according to creatinine clearance (CrCl), CockGroft-Gault equation, modification of diet in renal disease (MDRD) and chronic kidney disease-epidemiology collaboration (CKD-EPI). CrCl in 24-hr urine collection is expressed using urine creatinine (mg per deciliter or micromole per liter) multiplication by urine volume (milliliter or liter) divided on plasma creatinine (milligram per deciliter or micromole per liter) multiplied 1440 and its unit is expressed with milliliter per minutes (ml/min). Cockcroft-Gault equation is expressed as CrCl = (140 – age) × wt divided on SCr × 72, multiplication by 0.85 if female. MDRD equation given by: estima–ted GFR = 175 × Standardized SCr–1.154 × age–0.203 × 1.212 [if black] × 0.742 [if female] where eGFR is expressed as ml/min/1.73 m2 of body surface area and SCr is expressed as mg per dl. The CKD-EPI equation, expressed as a single equation, is eGFR = 141 × min (Scr/κ,1)α × max (Scr/κ, 1) – 1.209 × 0.993age × 1.018 [if female] – 1.159 [if black], where κ is 0.7 for females and 0.9 for males, α is –0.329 for females and 0.411 for males, min indicates the minimum Scr/k or 1 and max indicates the maximum of Scr/κ or 1. Proteinuria, albumin-to-creatinine ratio (ACR) is greater than 2.5 mg/mmol in men or 3.5 mg/mmol in women, or a protein-to-creatinine ratio (PCR) is greater than 15 mg/mmol is sufficient for diagnosis of CKD (random PCR < 15 mg/mmol: normal; 15–49 mg/mmol: trace proteinuria; 50–99 mg/mmol: significant proteinuria; 100–300 mg/mmol: high proteinuria; > 300 mg/mmol: nephrotic range proteinuria). Albuminuria may be classified as moderately increased albuminuria (3–30 mg/mmol creatinine) or severely increased albuminuria (greater than 30 mg/mmol creatinine). The normal PCR in children and adolescent is less than 0.3. In infants and younger children, the PCR is higher with the upper normal limit of 0.5. PCR above 3 is found in patients with nephrotic syndrome. The daily protein excretion rate (PER) can be determined from spot urine PCR, based on sex, age and weight using the following equations: PER (g/m2/day) = 0.63* (PCR).
Markers of fibrillary glomerulonephritis
DNAjB9 is a 223-aminoacid protein that is a member of the DNAj family of chaperons with a predicted 23-aminoacid signal peptide. It is a heat shock protein in ER/unfolded response pathway and binds to aggregation-prone peptides. DNAjB9 is present in glomerular and extraglomerular immune deposits of patients with fibrillary glomerulopathy [6]. DNAJ proteins influence on many of cellular processes by regulating the ATPase activity of 70-kD heat shock proteins. DNAjB9 is involved in ER stress and the UPR and it is a cochaperone for Bip/Grp78, a master regulator of the URP. DNAJB9 is upregulated by ER stress, nitric oxide and other inflammatory mediators, protects against cell death, protects hematopoietic stem cells during stress and is required for normal B cell development and antibody production. DNAJB9 also specifically binds aggregation-prone regions in proteins. Methods for detecting DNAjB9 marker in kidney biopsy specimens are by liquid chromatography/tandem mass spectrometry and laser microdissection-assisted shotgun proteomics [7]. DNAjB9 is a useful diagnostic marker for diagnosis of atypical forms of fibrillary glomerulopathy. Patients patients with fibrillary glomerulonephritis were classified into groups I and II in the current research. Group I was considered as DNAjB9-positive tissue and group II was considered as DNAjB9-negative tissue in biopsy-proven kidney specimens.
Definition of normal values of serum protein electrophoresis (SPEP), urine protein electrophoresis (UPEP), serum immunoelectrophoresis (SIEP), urine immunoelectrophoresis (UIEP), serum immune fixation (SIF), and urine immune fixation (UIF)
The monoclonal components are usually identified and quantified by electrophoresis and immunofixation of serum (SPE + sIFE) and urine (UPE + uIFE) proteins. Normal range for serum immunoglobulins in SIEP are defined with serum immunoglobulin A (IgA) of 70–350 mg/dl, immunoglobulin D (IgD) of 0–14 mg/dl, immunoglobulin E (IgE) of 1–87 IU/ml, immunoglobulin G (IgG) of 700–1700 mg/dl (IgG1of 270–1740 mg/dl; IgG2 of 30–630 mg/dl; IgG3 of 13–320 mg/dl; IgG4 of 11–620 mg/dl) and immunoglo–bulin M (IgM) of 50–300 mg/dl. In serum and urine protein electrophoresis, normal value for albumin is defined 3.5–5.5 (50–60 %), globulin 2–3.5 g/dl (40–50 %), alpha1 0.2–0.4 g/dl (4.2–7.2 %), alpha2 0.5–0.9 g/dl (6.8–12 %), beta 0.6–1.1 g/dl (9.3–15 %) and gamma globulin is 0.7–1.7 g/dl (13–23 %). Normal range for serum free light chain kappa (sFLCκ) level is 3.3 to19.4 mg/l, for serum free light chain lambda (sFLCλ) level is 5.7 to 26 mg/dl, for kappa to lambda ratio is 0.26 to 1.65 in one reference and in other reference 1.47–2.95. Reference range of ratio in this article has been considered 0.26 to 1.65. Normal value for urine free light chain kappa (uFLCκ) is considered < 2.5 mg/dl and for urine free light chain lambda (uFLCλ) levels is defined < 5 mg/dl. Normal value for urine bence jones protein is considered undetectable. Normal serum beta-2 microglobulin (β-2 MG) is considered 0.7–1.8 mg/l and 1.1 to 2.4 mg/l in male and female, respectively. Normal 24-hr urine excretion of β-2 MG is mentioned < 120 μg/day and normal concentration of urinary β-2 MG is reported less than 300 μg/l in scientific references. Free heavy chains are called α, δ, ε, ϒ, μ and normal values for these subtypes is defined negative.
Definition of normal values of autoantibodies and complement system
Normal range of complement 3 (C3) is considered 88–201 mg/dl and normal range for complement 4 (C4) is defined 16–48 mg/dl or 0.16 to 0.48 gram per liter. Fifty percent hemolytic complement (CH50) level is defined 150 to 250 units per milliliter. Serum factor H (FH) autoantibody is defined 0.3 to 0.6 g/l and as percent normal range for it is defined 0–7.3 %. Serum Factor B (FB) level is in range of 17–22 mg/dl. Positive anti-nuclear antibodies is defined more than or equal to 1 over 160 titer and positive anti-double stranded deoxynucleic acids antibodies (Anti-DS DNA Abs) is considered more than or equal 1 over 10. Normal levels of autoantibodies are considered for cytoplasmic antineutrophil cytoplasmic antibodies (C-ANCA) < 2.8 unit over milliliter (U/ml), perinuclear antineutrophil cytoplasmic antibodies (P-ANCA) < 1.4 U/ml, anti-glomerular basement membrane antibodies (anti-GBM Abs) < 5U/ml, anti-parietal cell antibody at 1over 20 (1 : 20) titer and anti-smooth muscle antibody titer of 1/20. Normal ranges for anti-mitochondrial antibody titer, anti-smith antibody, anti-ribonucleoprotein antibody (anti-RNP), anti-Scl 70 antibody (anti-topoisomerase I), anti-platelet antibody, anti-R0 antibody, anti-Jo-1 antibody (anti-histidyl) and anti-La antibody are considered negative. Normal value for serum rheumatoid factor and anti-citrulinated peptide/protein antibodies (ACPA) such as anti-cyclic citrulinated peptide antibody (anti-CCP) is considered < 30 IU/ml and < 20 Unit, respectively. Reference Range in UpToDate for Anti-CCP antibody is considered level < 20 EU/ml (negative), 20–39 EU/ml (weakly positive), 40–59 EU/mL (moderately positive), > 60 EU/mL (strongly positive or at least three times the upper limit of normal). Another alternative test for anti-CCP antibody is called anti-mutated citrulinated vimentin.
Definition of non-albumin proteinuria (NAP)
NAP is calculated as non-albumin protein to creatinine ratio (NAPCR) is equal with urinary protein to creatinine ratio (UPCR) minus urinary albumin to creatinine ratio (UACR). Cut-off value for NAP is 120 mg/g and isolated NAP (iNAP) is defined with UPCR ≥ 150 mg/g and UACR < 30 mg/g. NAP is used as complementary diabetic kidney disease (DKD) marker to albuminuria. Researchers found NAP was significantly associated with CKD progression that defined as decline in CKD stage with decrease of ≥ 25 % in eGFR from the baseline [8].
Assessment of risk of bias and quality in included articles
Case reports were analyzed using criteria developed by the Joanna Briggs Institute Critical Appraisal tool for case reports that has different assessment tools for each study design in question. The evaluation tool has 8 items for case reports.
Statistical analysis
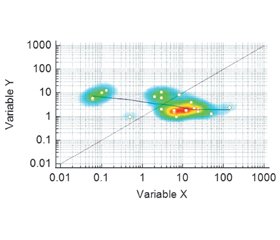
Data were entered in Microsoft Excel 2010 software. Categorical variables are recorded as frequency (N) and percentage (%). The continuous variables were determined as to whether they were normally distributed using the Kolmogorove-Smirnov or Shapiro-Wilk test. Continuous variables with normal distribution reported as mean ± standard deviation (SD). Nonparametric variables are expressed as median and interquartile range (Q1, Q3 and IQR). Comparisons between continuous variables with normally distributed (ND) data assessed by two-tailed t test analysis. Effect size of variable on outcome was analyzed using two proportion meta-analysis. Kaplan-Miere analysis was used for mortality probability. Correlation between two non-parametric variables were assessed using spearman’s tests. Moreover, relative risk and odds ratio for statistical analyses were used. Significance was assessed with p-value of < 0.05.
Results
Description of studies
Results of the search and study selection
Author identified 3045 records after searching electronic databases. Alongside, five articles were removed (N = 5) and total 3040 titles and abstracts identified. Then 3040 articles screened and author discarded 2974 full-texts articles due to non-related subject. Thereafter 66 articles were eligible and 4 articles were discarded due to non-case reports. Of these, 62 published articles (72 case reports) were included and enrolled as participants in this study.
Included studies (criteria)
Sixty-two published articles (72 case reports or participants) were considered for inclusion in this research.
Study characteristics
Study design
This research categorized as analytic (experimental) prospective study type with randomized control trials (RCTs) design in systematic review and meta-analysis article. Retrospective data were collected via electronic method in this research.
Sample sizes
Sample sizes of 72 patients or participants were considered in this study.
Setting
Participants were referred to single center or multi-center settings (emergency room or hospital or clinic) in this research.
Participants
All patients with biopsy-proven kidney specimens infavor of fibrillary GP included in this study. In those patients, structural or functional marker for kidney damage such as elevated serum creatinine levels or decreased eGFR, significant proteinuria and active urinalysis were noticed. Moreover, staining for DNAjB9 protein in kidney specimens was done.
Excluded studies (criteria)
Patients were excluded from the study if they were suspected to or not diagnosed as fibrillary glomerulopathy in kidney biopsy at initial time or during follow up except in one case report that kidney biopsy was not performed due to death in familial fibrillary glomerulonephritis (father) and DNAjB9 marker was not performed in two brothers. So it was supposed that each three case be put in DNAjB9 negative groups.
Risk of bias and quality in the included studies
Assessment of risk of bias and quality of included articles performed using Joanna Briggs Institute critical appraisal tools for case reports. Based on these criteria, six out of seventy-two case reports obtained eight score (6/72, 8.3 %), fifty out of seventy-two case reports had seven score (50/72, 69.4 %), twelve out of seventy-two case reports achieved to six score (12/72,16.6 %), three out of seventy-two patient attained five score (3/72, 4.1 %) and one out of seventy-two patients reach to three score (1/72, 1.3 %).
Results of case studies
Patients’ Characteristics
Among 3045 full-text articles obtained in this research paper, five articles deduplicated and total 3040 articles identified. In current research, 3040 articles screened and 2974 articles were excluded due to unrelated subject, review articles and other studies. Then 66 full-text articles were eligible and 4 articles were excluded due to non-case reports (n = 4). Finally 62 published articles that contained 72 participants were included in this study because one published article may contain more than one case report (Fig. 1). The sixty-two published articles (examined seventy-two case reports) were interrogated clinical, laboratory, imaging data and biopsy-proven kidney specimens of patients with fibrillary glomerulopathy in the current research [9–70]. Forty out of seventy-two patients were male (40/72, 55.5 %) and thirty-two of them female (32/72, 44.4 %). Eight of seventy-two patients (8/72, 11.1 %) were Caucasian, six of seventy-two patients (6/72, 8.3 %) belonged to white descent, four out of seventy-two patients (4/72, 5.5 %) were Japanese and African American ethnicity, one out of seventy-one (1/72, 1.3 %) belonged to Korean race and Non-Hispanic ethnicity. The median and IQR of age of patients with fibrillary nephropathy at time of diagnosis was 55 and 18 years old, respectively. The mean average of age in male and female patients were 53.55 ± 13.78 and 56.29 ± 15.8 years old (range from 1 to 80 years) respectively. There were no statistical significant level between two sex groups in current research (p-value: 0.35).
/40.jpg)
Patients’ Complains
The patients with fibrillary glomerulopathy were presented with various symptoms. These symptoms comprise lower leg extremity edema in seventeen out of seventy-two patients (17/72, 23.6 %), nausea and dyspnea in six out of seventy-two patients (6/72, 8.3 %), abdominal pain and headache in four out of seventy-two patients (4/72, 5.5 %). Twenty-seven out of seventy-two patients (27/72, 37.5 %) had history of hypertension and fourteen out of seventy-two patients (14/72, 19.4 %) referred with history of diabetes mellitus. Seven out of seventy-two patients with fibrillary glomerulopathy (7/72, 9.7 %) had history of obesity. Four out of seventy-two patients (4/72, 5.5 %) gave history of smoking and three out of seventy-two patients (3/72, 4.1 %) patients had history of dyslipidemia, weakness and asthenia in the current research. Two out of seventy-two patients (2/72, 2.7 %) had history of gastroesophageal reflux disorders (GERD), weight gain, loss of appetite, red-colored urine, skin lesions, pale conjunctiva and ankle swelling. In sign of patients with fibrillary glomerulopathy, twenty-four out of seventy-two patients (24/72, 33.3 %) were manifested with hypertension and fourteen of seventy-two patients (14/72, 19.4 %) presented with lower extremity edema. Four out of seventy-two patients with fibrillary glomerulopathy (4/72, 5.5 %) revealed abnormal chest auscultation, obesity and three out of seventy-two patients (3/72, 4.1 %) showed high temperature. Two out of seventy-two patients (2/72, 2.7 %) showed abnormal general appearance and one out of seventy-two patients (1/72, 1.3 %) developed overweight.
Laboratory data
In fifty-six out of seventy-two patients (56/72, 77.7 %) was performed urinalysis. Proteinuria was found in thirty-five out of fifty-six patients (35/56, 62.5 %) and nephrotic-range proteinuria detected in two out of thirty-five patients (2/35, 5.7 %) in dipstick. Red blood cells detected in forty-eight of fifty-six patients (48/56, 85.7 %) and occult blood found in three out of fifty-six patients (3/56, 5.3 %) in urinalysis. Dysmorphic red blood cell (RBC) found in five out of forty-eight patients (5/48, 10.4 %) in urine of patients in current study. Pyuria was measured in twelve out of fifty-six patients (12/56, 21.4 %) and significant pyuria was seen in six out of twelve (6/12, 50 %). Urine eosinophil more than 5 percent found in one out of twelve patients (1/12, 8.3 %) in urinalysis. Granular cast was found in six out of fifty-six patients (6/56, 10.7 %), hyalin cast in five out of fifty-six patients (5/56, 8.9 %), fatty and RBC cast in two out of fifty-six patients (2/56, 3.5 %), oval fat body cast and waxy cast in one out of fifty-six patients (1/56, 1.7 %) in urinalysis. Urine epithelial cells were seen in one out of fifty-six patients (1/56, 1.7 %) in dipstick. Serum creatinine was measured in sixty-seven out of seventy-two patients (67/72, 93 %) and elevated SCr was seen in forty-nine out of sixty-seven patients (49/67, 73.1 %) with median of 2.17 and IQR of 1.86 mg/dl (Q3-Q1 = 3.55–1.69). Blood urea nitrogen was measured in twenty-four of seventy-two of patients (24/72, 33.3 %) and elevated serum blood urea nitrogen was seen in seventeen of twenty-four patients (17/24, 70.8 %) with median of 39.2 and IQR of 62.7 mg/dl. Serum urea was measured in seven out of seventy-two patients (7/72, 9.7 %) and five of seven patients (5/7, 71.4 %) revealed elevated serum urea with the mean average of 89.96 ± 35.34 mg/dl. Estimated GFR was measured in fifteen out of seventy-two patients (15/72, 20.8 %) and decreased eGFR was seen in thirteen of fifteen patients with fibrillary glomerulopathy (13/15, 86.6 %) with the mean average of 58.83 ± 16.99 ml/min/1.73 m2 in the present research. Serum hemoglobin was measured in twenty-four of seventy-two patients (24/72, 33.3 %) that anemia was seen in twenty-two patients (22/24, 91.6 %) with the mean average of 9.52 ± 1.92 g/dl. Leukocyte count was measured in twenty-two out of seventy-two patients (22/72, 30.5 %) and leukocytosis was observed in five out of twenty-two patients (5/22, 22.7 %) with the mean average of 15 450 ± 3971.46 cells/103. Two out of twenty-two patients (2/22, 9 %) had leukopenia with the mean average of 4040 ± 130 cells/103 in the present research. Platelets count was measured in twenty out of seventy-two patients (20/72, 27.7 %) and thrombocytopenia was seen in two out of twenty patients (2/20, 10 %) with the mean average of 70 850 ± 45 860.08 cells/103. Serum albumin was measured in thirty-seven out of seventy-two patients (37/72, 51.3 %) and hypoalbuminemia (serum albumin < 3.5–4 g/dl) has been seen in twenty-eight out of thirty-seven patients (28/37, 75.6 %) with the mean average of 2.61 ± 0.48 g/dl with fibrillary glomerulopathy in the present research. Erythrocyte sedimentation rate (ESR) was measured in ten out of seventy-two patients (10/72, 13.8 %) and elevated erythrocyte sedimentation rate (ESR) was seen in eight out of ten patients (8/10, 80 %) with the mean average of 48.44 ± 27.22 mm/hr in current research. 24-hr urine protein was measured in fifty-eight out of seventy-two patients (58/72, 80.5 %) and fifty-seven out of fifty-eight patients (57/58, 98.2 %) showed significant proteinuria with the median of 4200 mg and IQR of 5900 mg (Q3-Q1 = 8000–2100) in 24-hrs. Spot UPCR was measured in sixteen out of seventy-two patients (16/72, 22.2 %) and elevated spot urine protein to creatinine ratio was seen in fifteen of sixteen patients (15/16, 93.7 %) with the mean average of 3924.25 ± 2556.76 mg/g in the present research. Non-albumin PCR (NAPCR) with value of 2083.91 mg/g found in one out of seventy-two patients (1/72, 1.3 %) and elevated NAPCR was seen in 100 % of patients in current research. DNAjB9 detected in eight of seventy-two patients (8/72, 11.1 %) that two out of eight patients (2/8, 25 %) found in kidney renal recipients and six out of eight patients (6/8, 75 %) found in non-transplant patients. Serum protein electrophoresis was measured in thirty-four out of seventy-two patients (34/72, 29.4 %) and abnormal serum protein electrophoresis was seen in ten out of seventy-two patients (10/34, 13.8 %). There are low gamma fraction in two out of twenty-four patients (2/24, 8.3 %) in protein electrophoresis in current research. UPEP was measured in sixteen out of seventy-two patients (16/72, 22.2 %) and there was abnormal urine protein electrophoresis in four out of sixteen (4/16, 25 %) in current research. Serum IgG in SIEP was measured in eleven out of seventy-two patients (11/72, 15.2 %) in the present research. Elevated immunoglobulin (IgG) levels were seen in two out of eleven patients (2/11, 18.1 %) and low IgG levels were seen in three out of eleven patients (3/11, 2.7 %) in the current research. Serum IgM in SIEP was measured in ten out of seventy-two patients (10/72, 13.8 %) in current research. Elevated serum IgM levels were seen in three out of ten patients (3/10, 3 %) and low IgM levels was seen in one out of ten patients (1/10, 10 %) in the present research. In this research, SIF was measured in thirty-six out of seventy-two patients (36/72, 50 %) and there are abnormal serum immunofixation in ten out of thirty-six patients (10/36, 27.7 %). Serum free kappa levels in SIF was measured in seven out of seventy-two patients (7/72, 9.7 %) and there are elevated free kappa levels in seven out seven (7/7, 100 %) with median of 1000 and IQR of 3320.73 mg/l. Serum free lambda levels in SIF was measured in six out of seventy-two patients (6/72, 8.3 %) and elevated free lambda levels was seen in five out six patients (5/6, 83.3 %) with the mean average of 95.26 ± 70.71 mg/l. Free kappa to lambda levels was measured in nine out of seventy-two patients (9/72, 12.5 %) and high free kappa to lambda levels (κ/λ ratio) was seen in three out of nine patients (3/9, 33.3 %) with the mean average of 3.82 ± 2.26 in the present research. UIF was measured in thirty out of seventy-two patients (30/72, 41.6 %) and there are abnormal UIF in nine out of thirty patients (9/30, 30 %) in the present research. Anti-HCV antibody was measured in ten out of seventy-two patients (10/72, 13.8 %) and positive anti-HCV Ab was seen in five out of ten patients (5/10, 50 %) in the present research. HCV RNA PCR was measured in three out of seventy-two patients (3/72, 4.1 %) and positive HCV RNA PCR were seen in two out of three patients (2/3, 66.6 %) in current research. ANA was measured in thirty-seven out of seventy-two patients (37/72, 51.3 %) and there is positive anti-nuclear antibody titer (≥ 160) in six out of thirty-seven patients (6/37, 16.2 %) with median of 1/320 and the IQR of 1 to 320 titer in the present research. C-ANCA was measured in sixteen out of seventy-two patients (16/72, 22.2 %) and P-ANCA was measured in seventeen out of seventy-two patients (17/72, 23.6 %) in current research. Positive C-ANCA was seen in one out of sixteen patients (1/16, 6.25 %) and C-ANCA was seen in one out of seventeen patients (1/17, 5.8 %). Anti-GBM antibody was measured in eleven out of seventy-two patients (11/72, 15.2 %) and positive test was seen in two out of eleven patients (2/11, 18.1 %) in current research. Serum C3 level was measured in forty-four out of seventy-two patients (44/72, 61.1 %) and there is low C3 in nine out of forty-four patients (9/44, 20.4 %) in current research. Serum C4 level was measured in forty-two out of seventy-two patients (42/72, 58.3 %) and low C4 level in three out of forty-two patients (3/42, 7.1 %) in current research. Serum CH50 level was seen in five out of seventy-two patients (5/72, 6.9 %) and decreased CH50 level was seen in three out of five patients (3/5, 60 %) with the mean average of 32.56 ± 10.39 mg/l. High Factor H antibody was measured in two out of seventy-two patients (2/72, 2.7 %) and elevated FH antibody level was seen in one out of two patients (1/2, 50 %) in the present research. Serum CRP level was measured in six out of seventy-two patients (6/72, 8.3 %) and high CRP was seen in five out of six patients (5/6, 83.3 %) patients with median and IQR of 5.9 and 8162.65 mg/l, respectively. Serum β-2 microglobulin level was measured in two out of seventy-two patients (2/72, 2.7 %) and elevated β-2 microglobulin was in two out of two patients (2/2, 100 %) with the mean average of 1000.65 ± 995.35 mg/l. Urinary β-2 microglobulin concentration was measured in one out of seventy-two patients (1/72, 1.3 %) and elevated urinary β-2 microglobulin concentration was seen in one out of one patient (1/1,100 %) in current research. M-spike was seen in two of seventy-two patients (2/72, 2.7 %) with the mean average of 1159.5 ± 1140.5 mg/l. Creatinine clearance (CrCl) was measured in fifteen out of seventy-two patients (15/72, 20.8 %) in current research. There were decreased creatinine clearance in eight of out fifteen patients (8/15, 53.3 %) with median and IQR of 27 and 37 ml/min/1.73 m2, respectively. Elevated creatinine clearance was seen in two out of fifteen patients (2/15, 13.3 %) with the mean average of 121.7 ± 21.4 ml/min/1.73 m2 in the present research. eGFR was measured in fifteen out of seventy-two patients (15/72, 20.8 %) and decreased estimated glomerular filtration rate (eGFR) was seen in thirteen out seventy-two patients (13/15, 86.6 %) with the mean average of 58.80 ± 16.99 ml/min/1.73 m2 in the present research. There was raised eGFR in two out of fifteen patients (2/15, 13.3 %) with the mean average of 111.45 ± 3.25 ml/min/1.73 m2 in the current research. Serum blood sugar was measured in four out of seventy-two patients (4/72, 5.5 %) that there was hypoglycemia and hyperglycemia in one out four patients (1/4, 25 %) patients in the current research. Serum chloride was measured in six out of seventy-two patients (6/72, 8.3 %) and hyperchloremia was seen in three out of six patients (3/6, 50 %) with the mean average of 112.30 ± 3.39 mEq/l. Lower limit of normal range for serum chloride was seen in one out of six patients (1/6, 16.6 %) in the present research. Serum uric acid was measured in six out of seventy-two patients (6/72, 8.3 %) and there was hyperuricemia in four out of six patients (4/6, 66.6 %) with the mean average of 8.85 ± 0.85 mg/dl in the present research. Serum sodium was measured in seven out of seventy-two patients (7/72, 9.7 %) and hyponatremia was seen in two out of seven patients (2/7, 28.5 %) with the mean average of 130.25 ± 1.75 mEq/l in current research. Serum potassium was measured in eight out of seventy-two patients (8/72, 11.1 %) and hyperkalemia were seen in two out of eight patients (2/8, 25 %) with the mean average of 6.42 ± 0.42 mEq/l in current research. Serum transaminases were measured in eleven out of seventy-two patients (11/72, 15.2 %). Elevated aminotransferase above 22 IU/l were seen in six out of ele–ven patients (6/11, 54.5 %) with median of 37.5 IU/l and IQR of 40 IU/l for AST, median of 43 and IQR of 41 IU/l for ALT in current research. Serum cholesterol was measured in nineteen out of seventy-two patients (19/72, 26.3 %) in current research. There was elevated total cholesterol in thirteen out of nineteen (13/19, 68.4 %) with median of 247 mg/dl and IQR of 126 mg/dl. Fibril size was measured in sixty-nine out of seventy-two patients (69/72, 83.3 %) with median size of 15 nm and IQR of 6.5 nm –(Q3-Q1 = 18.5–12.4) in the present research.
Pathologic findings
Working group updated oxford classification of IgA nephropathy in 2016 year and five parameters of MEST-C score were considered for this classification. Based on this workshop, kidney specimens must contain at least eight glomeruli number. Number of glomeruli with endocapillary hypercellularity, necrosis, extracapillary hypercellularity (cellular/fibrocellular crescents), global glomerulosclerosis and segmental glomerulosclerosis in this classification must be considered (Fig. 2).
/43.jpg)
Kidney biopsy was performed in seventy-one out of seventy-two patients (71/72, 98.6 %) in the present research. Kidney biopsy was not performed in one patient (1/72, 1.3 %) due to death in current research. According to Oxford MEST-C classification, there was M0 score in twenty-two of seventy-one patients (22/71, 30.9 %), M1 score in four out of seventy-one patients (4/71, 5.6 %), undetermined mesangial score in eight out of seventy-one patients (8/71, 11.2 %) in current research. E1 score found in fifteen out of seventy-one patients (15/71, 21.1 %), E0 in three out of seventy-one patients (3/71, 4.2 %) and undetermined E score in one out of seventy-one patients (1/72, 1.3 %) in the present research. There was C2 in eight out of seventy-one patients (8/71, 11.2 %), C1 in five out of seventy-one patients (5/71, 7 %) and three out of seventy-one patients (3/71, 4.2 %) in current research. S1 found in thirty-nine out of seventy-one patients (39/71, 54.9 %) in the present research. T0 found in thirty of seventy-one patients (30/71, 41.7 %), T1 in nine out of seventy-one patients (9/71, 12.6 %), T2 in seven out of seventy-one patients (7/71, 9.8 %) in current research. Double contour glomerular basement membrane (GBM) detected in six out of seventy-one patients (6/71, 8.4 %) and DNAjB9 marker found in kidney biopsies of eight out of seventy-one patients (8/71, 11.2 %) in current research. In renal allograft recipients, there was mm0 in two out of seventy-one patients (2/71, 2.8 %), i1, t1, v0, g1, ptc3, c4d3, ci0, cv1, cv3, cg1b, mm3 in one out of seventy-one patients (1/71, 1.4 %) patients in current research. Undetermined ci, cv, ct and mm and mesangial proliferation found in one out of seventy-one patients (1/71, 1.4%) in the present research (Table 1).
/44.jpg)
/45.jpg)
/46.jpg)
/47.jpg)
Imaging techniques
Chest x-ray in the present research revealed different abnormalities such as bilateral pleural effusion in two out of seventy-two patients (2/72, 2.7 %), bulky left hilum, bilateral cottony interstitial infiltrates, mild interstitial lung disease (ILD), diffuse interstitial process and atelectasis of left lower lobe, mild cardiomegaly in one out of seventy-two patients (1/72, 1.3 %) in current research. Abnormal kidney ultrasonography was seen in thirteen out of seventy-two patients (13/72, 18 %) in current research. There were various kidney abnormalities in ultrasonography as increased parenchymal echogenicity, scattered cyst, simple cyst, enlarged kidney sizes, bilateral small kidney, single kidney with compensatory hypertrophy of other kidney, enlarged kidneys with multiple cyst, bilateral kidneys with increased echogenicity and irregular surface, bilateral kidneys with increased echogenicity, irregular surface and normal sizes in the present research. A small benign cyst was seen in ultrasound scan of one out of seventy-one patients (1/72, 1.3 %) in the present research. Abdominal sonography in one out of seventy-two patients (1/72, 1.3 %) revealed ascites, gall bladder stone and bilateral pleural effusion. Upper GI endoscopy was performed in two out of seventy-two patients (2/72, 2.7 %) that in one case (1/72, 1.3 %) revealed macroscopic evidence of gastritis with polypoid mass and central ulceration on the anterior wall of the stomach. Another case showed chronic antral gastritis and duodenitis with superficial erosions. Two abnormal findings were seen in echocardiography (2/72, 2.7 %) as mild mitral regurgitation (MR) and slight left ventricular hypertrophy (LVH) in the present research. Chest computed tomography (CT) scan in one out of seventy-two patients (1/72, 1.3 %) revealed bilateral interstitial pulmonary infiltration and abdominal CT scan showed renal atrophy, ascites and multiple liver abscesses.
Treatment modalities
Therapeutic modalities comprise oral steroids in forty-two out of seventy-two patients (42/72, 58.3 %), IV methylprednisolone in thirty-two out of seventy-two patients (32/72, 44.4 %), immunosuppressive agents in forty patients (40/72, 55.5 %) that include cyclophosphamide (CPA) in fifteen cases (15/40, 37.5 %), azathioprine in eight cases (8/40, 20 %), cyclosporin in five cases (5/40, 12.5 %), mycophenolate mofetil (MMF) in four cases (4/40, 10 %), tacrolimus, chlorambucil and undetermined immunosuppressive agents in three cases (3/40, 7.5 %), sirolimus in 1 case (1/40, 2.5 %). Rituximab was used in ten out of seventy-two patients (10/72, 13.8 %) and plasmapheresis in seven out of seventy-two patients (7/72, 9.7 %). Interferons were used in three out of seventy-two patients (3/72, 4.1 %) that consist interferon, interferon alpha and interferon alpha 2A. Immunoglobulins were used in three out of seventy-two patients (3/72, 4.1 %) in the present research. Angiotensin-converting enzyme inhibitors (ACEIs) were used in twenty-five out of seventy-two patients (25/72, 34.7 %), angiotensin receptor blockers (ARBs) were used in eight out of seventy-two patients (8/72, 15.2 %) and dual renin angiotensin system (RAS) blockades in three out of seventy-two patients (3/72, 4.1 %). Diuretics were consumed in fourteen out of seventy-two patients (14/72, 19.4 %). Calcium channel blockers were used in eight out of seventy-two patients (8/72, 11.1 %) and beta-blockers in four out of seventy-two patients (4/72, 5.5 %). H2-blockers were used in four out of seventy-two patients (4/72, 5.5 %) patients with fibrillary glomerulopathy. Fifteen out of seventy-two patients (15/72, 20.3 %) underwent hemodialysis (HD) in current research and two out of seventy-two patients (2/72, 2.7 %) underwent peritoneal dialysis (PD). Undetermined dialysis (2/72, 2.7 %) performed in one out of seventy-two patients (1/72, 1.3 %) in the present research.
Outcomes and follow up
Characteristics of patients during follow up has been recorded in Table S8 in current research.
Primary end-points
Serum creatinine was measured in forty out of seventy-two patients (40/72, 55.5 %) and in accordance with SCr, three out of forty patients (3/40, 7.5 %) found AKI, four out of forty patients (4/40, 10 %) found AKD, fourteen out of forty patients (14/40, 35 %) developed CKD during follow up in current research. NKD found in one out of forty patients (1/40, 2.5 %) based on eGFR calculation. Elevated SCr was seen in twenty-eight out of forty patients (28/40, 70 %) with median of 2.18 mg/dl and IQR of 4 mg/dl (Q3-Q1 = 5.65–1.55) during time of follow up (time of the last serum creatinine measurement) in the present research. There was significant statistical correlation between elevated SCr and follow up time with p value of 0.01 and confidence interval of 0.7820 to 0.1258 during follow up (Fig. 3). Relative risk of kidney failure progression to KRT (≥ 2 fold elevation in SCr or dialysis or kidney transplant) in exposed to DNAjB9 positive patients (Group I) and DNAjB9 negative patients (Group II) was assessed 2.67 with 95% CI of 1.128 to 6.3044 and p value of 0.025. Odds ratio of kidney failure progression to KRT (≥ 2 fold elevation in SCr or dialysis or kidney transplant) was assessed 4.33 with 95% CI of 0.9464 to 19.8417 and p value of 0.058 in current research (Table 2).
/50.jpg)
Twenty-two out of seventy-two patients (22/72, 30.5 %) stayed on dialysis and two out twenty patients (2/20, 10 %) underwent PD during follow up period. Kidney disturbation was occurred in the median time of 6.5 hours and IQR of 14.5 hrs (Q3-Q1 = 17.5–3). Serum Bun was measured in six out of seventy-two patients (6/72, 8.3 %) and three out of six patients (3/6, 50 %) found elevated blood urea nitrogen with the mean average of 69.0 ± 23.8 mg/dl in current research. Creatinine clearance was measured in three out of seventy-two patients (3/72, 4.1 %) and two out of three patients (2/3, 66.6 %) found decreased creatinine clearance with the mean average of 20.2 ± 11.5 milliliter per minute (cc/min). Estimated GFR was measured in five out of seventy-two patients (5/72, 6.9 %) and five out of five patients (5/5, 100 %) patients developed declined eGFR with the mean average of 42.02 ± 18.94 ml/min/1.73 m2 in current research. 24-hr urine protein collection was measured in twenty-one out of seventy-two patients (21/72, 29.1 %) and significant 24-hr proteinuria was seen in fourteen out of twenty-one patients (14/21, 66.6 %) with mean of 1.09 ± 0.75 g/24 hr in current research. UPCR was measured in nine out of seventy-two patients (9/72, 12.5 %) and eight out of nine patients (8/9, 88.8 %) developed elevated UPCR proteinuria with median of 800 mg/g and IQR of 12 600 mg/g (Q3-Q1 = 13 000–400) during follow up. Urinary bence jones protein (BJP) was measured in one out of seventy-two patients and elevated free BJP (free kappa protein) was seen in one out of one patient (1/1, 100 %) in the present research. Free kappa to lambda ratio was measured in two out of seventy-two patients (2/72, 2.7 %) and two out of two patients (2/2, 100 %) found elevated free kappa to lambda ratio in the present research. Eight out of seventy-two patients (8/72, 11.1 %) died in current research. Proportion of death in DNAjB9 positive patients (Group I) was assessed zero out of eight patients (0/8) and proportion of non-died patients in DNAjB9 positive patients was assessed eight out of eight patients (8/8,100 %). Proportion of death in DNAjB9 negative patients (Group II) was assessed eight out of sixty-four patients (8/64, 12.5 %) and proportion of non-died patients in DNAjB9 negative patients was assessed fifty-six out of sixty-four patients (56/64, 87.5 %) in current research. There was nonsignificant statistical level in comparison between DNAjB9-positive and DNAjB9-negative patients (proportion between two groups) during follow up in current meta-analysis (p = 0.29). There was statistical significant level at comparison between group I and group II for mortality probability (Kaplan-Miere analysis) during follow up in the present research (р < 0.0001) (Fig. 4).
/49.jpg)
KRT (renal transplant) was seen in four out of seventy-two patients (4/72, 5.5 %) in current research. Two out of eight DNAjB9 positive staining in kidney biopsy specimens found kidney transplantation (2/8, 25 %) and six out of eight DNAjB9 positive staining were not received kidney transplantation (6/8, 75 %). Proportion difference was assessed 21.9 % in this research. Comparison of these value was assessed 0.011 (p-value of 0.011) with confidence interval оf 2.51 to 56.05. Two out of sixty-four DNAjB9 negative staining in kidney biopsy specimens found kidney transplantation (2/64, 3.1 %) and sixty-two out of sixty-four DNAjB9 negative staining were not received kidney transplantation (62/64, 96.8 %). Two out of seventy-two patients (2/72, 2.7 %) developed recurrence of disease in fibrillary glomerulonephritis. Graft loss was seen in two out of four patients (2/4, 50 %) post-transplant period during follow up. There was not significant correlation between histologic marker of segmental glomerulosclerosis (S1) and DNAjB9 staining on kidney biopsy specimens (p-value of 0.11; correlation coefficient: 0.7).
Secondary end-points
Three out of seventy-two patients (3/72, 4.1 %) patients found ESKD in the present research. HCV RNA was measured in one out of seventy-two patients (1/72, 1.3 %) and it disappeared in one out of one patient (1/1, 100 %) during follow up. Herpers zoster was measured in one out seventy-two patients (1/72, 1.3 %) and found in one out one patient (100 %) in the present research. Serum transaminases were measured in two out of seventy-two patients (2/72, 2.7 %) and elevated serum transaminases found in one out of two patients (1/2, 50 %) in current research. C3 was measured in three out of seventy-two patients (3/72, 4.1 %) and low C3 was seen in one of three patients (1/3, 33.3 %) in current research. C4 was measured in two out of seventy-two patients patients (2/72, 2.7 %) and normal C4 detected in two out of two patients (2/2, 100 %). Platelet count was measured in two out of seventy-two patients and thrombocytopenia found in two out of two patients (100 %) in current research. Anti-nuclear antibodies was measured in one out of seventy-two patients (1/72, 1.3 %) and elevated ANA titer was seen in one out one patient (1/1, 100 %) in the present research.
Discussion
Fibrillary glomerulonephritis is a rare glomerular disease that has been found in less than 1 % of native kidney biopsies. This disease first described by Rosenmann and Eliakim in 1977 year [71]. Fibrillary GP is diagnosed by ultrastructural finding of arranged straight fibrils measuring to 10 to 30 nm in thickness in electron micro–scopy. Depositions in FGN are in the mesangium and GBM or both in electron microscopy. On immunofluorescence (IF) staining, the deposits stain for polyclonal IgG and complement indicating immune complex deposition. Somewhat ill-defined smudged deposits that stain most intensely for IgG, usually accompanied by C3, κ, λ and sometimes also associated with staining for C1q, IgM and/or IgA. In 5 % of cases, IF deposits stain by κ or λ but not both and such light chain restriction is related to dysproteinemia [3]. Morphologic features of FGN in IF staining consist mesangial expansion/hypercellularity with or without GBM duplication. Other morphologic features include endocapillary glomerulonephritis and crescentric glomerulonephritis. These patients present with proteinuria (most often with nephrotic syndrome), hematuria, renal insufficiency and hypertension that in 50 % of cases culminate in to end-stage kidney disease. In our research 19.4 % (14/72) of patients presented with lower leg extremity edema and 85.7 % (48/56) presented with microscopic hematuria. Clinical features of 33.3 % (24/72) of our patients were hypertension and there was proteinuria in one hundred (100%) patients. 33.3 % of our patients developed ESKD during 1 year follow up that was in disagreement with study by Andeen et al. that 53 % progressed to ESKD during 24 months follow up. DNAjB9 is a novel biomarker for FGN and DNAjB9 expression in the glomeruli is highly specific and sensitive for FGN. Whether serum DNAjB9 marker can be used for FGN or not, one study by Nasr et al. revealed that serum levels of DNAjB9 staining could be valuable marker to predict FGN with the complement kidney biopsy for the diagnosis of FGN [72]. Inherited FGN or familial FGN is reported in few cases and genetic background can play a role in pathogenesis of FGN because human leukocyte antigens (HLAs) involve in inherited risk factors for emerging FGN. HLA associated with FGN is seen in other kidney diseases. HLA-DR7 and HLA-DQ2 have been associated with steroid sensitive nephrotic syndrome and HLA-B-35 is seen in IgA nephropathy/Henoch-schoenline purpura (HSP) [73]. Moreover, association between FGN and HLAs have been reported as HLA-B35, HLA-DR-7 and DQ2 antigens. Lower frequency with HLA-DR4 has reported in FGN. Notably, association between hepatitis C virus infection and fibrillary glomerulonephritis has been reported in several studies. Positive HCV RNA PCR was seen in two out of three patients (2/3, 66.6 %) and positive anti-HCV Ab was seen in five out of ten patients (5/10, 50 %) in the present research that those values are approximately in agreement with stu–dies by Nasr et al. and Said et al. arisen positive hepatitis C infection. That study revealed positive Hepatitis C PCR in two out of forty-seven patients (2/47, 4.2 %) while study by said et al. revealed positive hepatitis C infection in one out of seventeen patients (1/17, 5.8 %) [74]. Association of this virus with FGN in black people in another study has been documented by Schober et al. that this value was higher in black people rather than white people [75]. Another finding in this research must be noticed that is age of patients with FGN. The median age of patients with FGN was 55 years old and there was slight male predominance (male to female ratio: 1.25) that was agreement with Study by Nasr et al. The mean age of patients at kidney biopsy was 53 years and female predominance was detected in that study. Another association of this disease has been reported with dysproteinemia and autoimmune diseases such as cryoglobulinemia and test for cryoglobulin must be performed before diagnosis of fibrillary GP. In our research, high free kappa and free lambda levels found in 100% (7/7) and 83.3 % (5/6) of patients with FGP, respectively. Moreover, high free kappa to lambda levels (κ/λ ratio) was seen in three out of nine patients (3/9, 33.3 %) with the mean average of 3.82 ± 2.26 in the present research. Two out of seventy-two patients (2/72, 2.7 %) had M-spike protein while in study by Nasr et al., was assessed eleven out of sixty-three patients (11/63, 17.4 %). Moreover, study by Marinaki et al. revealed negative monoclonal paraproteinemia, chronic viral infection and serologic tests for other autoimmune disorders in ten patients [76]. Positive ANA was seen in six out of thirty-seven patients (6/37, 16.2 %) and with median of 1/320 and the IQR of 1 to 320 titer and this value was disagreement with study by Said et al. that this value was assessed –higher (3/14, 21.4 %). Low C3 in nine out of forty-four patients (9/44, 20.4 %), low C4 in three of forty-two (3/42, 7.1 %) patients and low CH50 were seen in three out of five patients (3/5, 60 %) were detected while it was inconsistent with study by Said et al. that serum C3 and C4 were normal in all sixteen patients. Positive C-ANCA was seen in one out of sixteen patients (1/16, 6.25 %) and C-ANCA was seen in one out of seventeen patients (1/17, 5.8 %). Positive anti-GBM antibody was seen in two out of eleven patients (2/11, 18.1 %) in current research. Other finding in this research was presence of high relative risk and Odds ratio of fibrillary glomerulonephritis on outcome of kidney failure progression to KRT (persistent dialysis or kidney transplantation or ≥ 2-fold elevation in SCr) that assessed 2.67 and 4.33, respectively. The key points in this discussion are death probability in DNAjB9-negative patients and effect of this marker on outcomes of fibrillary glomerulonephritis. Survival probability of DNAjB9 negative patients with fibrillary GP was assessed 12.5 % vs. probability of 0 in DNAjB9-positive patients with significant statistical level (< 0.0001). Till to now based on my to my best knowledge, such study hasn’t been found in literature review and advanced searching. Because DNAjB9 is accounted as the fourth most abundant protein in FGN glomeruli, therefore can be said that it is the most common protein involving in its pathogenesis [77]. Hence it is possible that in the absence of ultrastructural evaluation (EM), this immunohistochemical marker can diagnose the fibrillary GN [3]. In conclusion, relative risk of kidney failure progression to KRT in exposed to DNAjB9 positive patients (Group I) and DNAjB9 negative patients (Group II) was assessed 2.67. There was statistical significant level at comparison between group I and group II for mortality probability (Kaplan-Miere analysis) during follow up in the present research.
Ethics Approval and consent to participate. Authors of published articles (case reports) stated that research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. They described that subjects (or their parents or guardians) were given their informed consent and study protocol was approved by the institute’s committee on human research.
Consent for publication. Not applicable.
Availability of data and material. Author put the dataset (supplementary data) with http://doi.org/10.6084/m9.figshare.20530224 in figshare repository after publication.
Acknowledgements. The author to wish thanks National University of Tehran Medical Sciences, College of Medicine and Imam Khomeini Hospital Complex. This paper has been written for medical students and higher degrees.
Dataset of manuscript entitled «Effect of FN1 mutation on outcomes of fibronectin glomerulopathy in a systematic review and meta-analysis» that has been published on 23 May 2022, located in figshare repository with Doi: 10.6084/m9.figshare.20532126.This repository is active.
Received 01.07.2022
Revised 18.07.2022
Accepted 26.07.2022
Список литературы
1. Kudose S., Canetta P., Andeen N.K. et al. Diagnostic approach to glomerulonephritis with fibrillar IgG deposits and light chain restriction. Kidney Int. Rep. 2021. 6. 936-45.
2. Rosenstock J.L., Markowitz G.S. Fibrillary glomerulonephritis: An update. Kidney Int. Rep. 2019. 4. 917-22.
3. Klomjit N., Alexander M.Р., Zand Ladan. Fibrillary Glomerulonephritis and DnaJ Homolog Subfamily B Member 9 (DNAJB9). Kidney360. 2020. 1. 1002-1013.
4. Ando M., Ohashi K., Akiyama H. et al. Chronic kidney disease in long term survivors of myeloablative allogenic haematopoietic cell transplantation: prevalence and risk factors. Nephrol. Dial. Transplant. 2010. 25. 278-82.
5. Hatamizadeh P. Introducing nephrocardiology. Clin. J. Am. Soc. Nephrol. 2022. 17. 311-3.
6. Andeen N.K., Yang H.Y., Dai D.F., MacCoss M.J., Smith J.D. Dnaj Homolog subfamily B member 9 is a putative autoantigen in fibrillary GN. J. Am. Soc. Nephrol. 2018. 29. 231-239.
7. Andeen N.K., Troxell M.L., Riazy M. et al. Fibrillary glomerulonephritis: clinicopathologic features and atypical cases from a multi-institutional Cohort. Clin. J. Am. Soc. Nephrol. 2019. 14. 1741-1750.
8. Bae J., Won Y.J., Lee B.W. Non-albumin proteinuria (NAP) as a complementary marker for diabetic kidney disease (DKD). Life. 2021. 11(224). 1-12.
9. Nasr S.Н., Chavez O., Dasari S., Thesis D.Т., Vrana J.А., Fatima H., et al. Donor-derived allect 2 amyloidosis and recurrent fibrillary glomerulonephritis in a transplant allograft. Kidney Med. 2021. 3(3). 433-37.
10. Park J.Н., Kim B.R., Chun B.G., Kim M.Н., Shin H.S., Jung Y.S. et al. Coexistence of fibrillary glomerulonephritis in a patient with multiple myeloma. Intern. Med. 2012. 51. 1379-1381.
11. Fisher P.W., Ho L.Т., Goldschmidt R., Semerdjian R.J., Rutecki G.W. Familial mediterranean fever, inflammation and nephrotic syndrome: fibrillary glomerulopathy and the M6801 missence mutation. BMC Nephrol. 2003. 41-7.
12. Javaid M.М., Denley H., Tagboto S. Fibrillary glomerulonephritis with small fibrils in a patient with the antiphospholipid antibody syndrome successfully treated with immunosuppressive therapy. BMC Nephrol. 2007. 8 (7). 1-6.
13. Pliquett R.U., Mohr P., Mukhtar B., Girndt M., Markau S. Plasmaphresis leading to remission of refractory nephrotic syndrome due to fibrillary glomerulonephritis: a case report. J. Med. Case Rep. 2012. 6. 116. 1-6.
14. Navaro-Antolin J., Quereda C., Mampaso F., Gonzalo A., Rivera M., Orte L. et al. Rapidly progressive fibrillary glomerulonephritis and cutaneous T-cell lymphoma. Nephron. 1996. 73. 107-8.
15. Adapa S., Konala V.М., Naramala S., Nast C.C. Multiple morphological phenotypes of monoclonal immunoglobulin disease on renal biopsy: significant of treatment. Clin. Nephrol. 2020. 8. 17-24.
16. Sung W.K., Jeong J.U., Bang K.T. et al. Fibrillary glomerulonephritis combined with chronic inflammatory demyelinating polyneuropathy. Kidney Res. Clin. Pract. 2015. 117-9.
17. Her M.Y., Kang M.S., Kim D.Y. Fibrillary glomerulonephritis in a patient with rheumatoid arthritis. Letters to Editors. Clin. Exp. Rheumatol. 2008. 26(1). 158.
18. Joffy S., Cathro H.Р., Bellizzi A.М., Balogun R.A. Renal clinico-pathology teaching case: Fibrillary glomerulonephritis. Tropical J. Nephrol. 2008. 3(2). 115-8.
19. Watanabe K., Nakai K., Hosokawa N. et al. A case of fibrillary glomerulonephritis with fibril deposition in the arteriolar wall and a family history of renal disease. Case Rep. Nephrol. Dial. 2017. 7. 26-33.
20. Fillippone E.J., Chmielewski C., Gulati R., Newman E., Faber J.L. Do novo fibrillary glomerulonephritis (FGN) in a renal transplant with chronic hepatitis B. Case Rep. Transpl. 2013. 1-5.
21. Lodhi M.U., Saleem T.S., Usman M.S. et al. Fibrillary glomerulonephritis in a patient with sjogren’s syndrome. Cureus. 2018. 10 (4). 1-7.
22. Gielen G.А.L., Wetzels J.F.M., Steenbergen E.J., Mudde A.H. Fibrillary glomerulonephritis in a patient with type 2 diabetes mellitus. Netherland J. Med. 2006. 64 (4). 119-123.
23. Jeyabalan A., Batal I., Piras D., Morris H.K., Appel G.B. Familial fibrillary glomerulonephritis in living related kidney transplantation. Kidney Int. Rep. 2021. 6. 239-42.
24. Momose A., Nakajima T., Chiba S. et al. A case of fibrillary glomerulonephritis associated with thrombotic microangiopathy and anti-glomerular basement membrane antibody. Nephron Extra. 2015. 5. 30-8.
25. Dolores Sánchez de la Nieta García M., González López L., Castro Fernández P. Fibrillary glomerulonephritis simulating glome–rular basal antimembrane antibody disease with associated thrombo–tic microangiopathy and ANCAp. Nefrologia. 2021. 907. 1-3.
26. Nebuloni M., Gendreni A., Tosoni A., Caruso S., di Belgiojoso G.B. Fibrillary glomerulonephritis with prevalent IgA deposition associated with undifferentiated connective tissue disease: A case report. Nephrol. Dial. Transplant. Plus. 2010. 3. 57-59.
27. Cheungpasitporn W., Zacharek C.С., Fervenza F.С., Cornell L.D., Sethi S., Herrera Hernandez L.Р. et al. Clin. Kidney J. 2016. 9 (1). 97-101.
28. Nilajgi S., Killen J.Р., Baer R., Renaut P., Mantha M. Fibrillary glomerulonephritis: presenting as crescentric glomerulonephritis causing rapidly progressive renal disease. Nephrol. Dial. Transplant. Plus. 2011. 4. 413-5.
29. Sethi S., Adeyi O.А., Rennke H.G. A case of fibrillary glomerulonephritis with linear immunoglobulin G staining of the glomerular capillary walls. Arch. Pathol. Lab. Med. 2001. 125. 534-6.
30. Kfoury H.K. Fibrillary glomerulonephritis: A diagnosis not to be missed. Saudi Kidney Dis. Transpl. 2021. 23 (6). 1246-50.
31. Shah H.Н., Thakkar J., Pullman J.М., Mathew A.T. Fibrillary glomerulonephritis presenting as crescentric glomerulonephritis. Indian J. Nephrol. 2017. 27 (2). 157-60.
32. Huerta A., Segovia B., Hernandez A. et al. When the finding of glomerular fibrils in patients with nephrotic syndrome leads to an erroneous diagnosis. Nephrol. Dial. Transplant. Plus. 2009. 2. 63-6.
33. Alpers C.Е., Kowalewska J. Fibrillary glomerulonephritis and immunotactoid glomerulopathy. J. Am. Soc. Nephrol. 2008. 19. 34-37.
34. Vera Mendez F.J., Molina Nunez M., Hernandez Garcia M.А., Garcia Solano J. Fibrillary and immunotactoid glomerulonephritis: report of a case and review of the literature. An. Med. Interna. 2005. 22(1). 35-8.
35. Marin L.L., Mendez R.В., Ferrer B.L. et al. Fibrillary glomerulonephritis: presentation of case and differential diagnostics with diseases from deposits. Morfovirtual 2016; Third Virtual Congress of Morphological Sciences. Third Scientific Conference of the Santiago Ramón y Cajal Chair. 1–15.
36. Churg J., Venkataseshan V.S. Fibrillary glomerulonephritis without immunoglobulin deposits in the kidney. Kidney Int. 1993. 44. 837-42.
37. Uchida T., Komatsu S., Sakai T., Kojima A., Iwama S., Sugisaki K., et al. CEN Case Rep. 2021. 10. 442-7.
38. Amir-Ansari B., O̕Donnell P., Nelson S.R., Cairns H.S. Fibrillary glomerulonephritis in a patient with adenocarcinoma of stomach. Nephrol. Dial. Transplant. 1999. 12. 210-11.
39. Lerner G., Singer G., Larsen C.Р., Caza T.N. Immunoglobulin-negative fibrillary glomerulonephritis masked in diabetic nephropathy: A case report and discussion of a diagnostic pitfall. Glomerular dis. 2021. 1-11.
40. Fernandez de Larrea C., Rovira M., Mascaro J.J.М. et al. Generalized cutis laxa and fibrillar glomerulopathy resulting from IgG deposition in IgG-lambda monoclonal gammopathy: pulmonary hemorrhage during stem cell mobilization and complete hematological response with bortezomib and dexamethasone therapy. Europ. J. Hematol. 2008. 82. 154-8.
41. Leibler C., Moktefi A., Matignon M., Debiais-Delpec C., Oniszczuk J., Sahali D. et al. Rituximab and fibrillary glomerulonephritis: Interest B cell reconstitution monitoring. J. Clin. Med. 2018. 7(430). 1-7.
42. Gandhi P., Tang J. Successful treatment of a unique case of congophilic fibrillary glomerulonephritis. Med. 2020. 99(28). 1-3.
43. Masson R.G., Rennke H.G., Gottlieb M.N. Pulmonary he–morrhage in a patient with fibrillary glomerulonephritis. New Engl. J. Med. 1992. 1-4.
44. Kornblihtt L.І., Vassaillu P.S., Heller P.G., Lago N.R., Alvarez C.L., Molinas F.S. Primary myelofibrosis in a patient who developed primary biliary cirrhosis, autoimmune hemolytic anemia and fibrillary glomerulonephritis. Ann. Hematol. 2008. 87. 1019-20.
45. Wu C.К., Leu J.G., Yang A.H., Tarng D.С., Tung H.Y., Chiang S.S. Simultaneous occurrence of fibrillary glomerulonephritis and renal fibrosis in nonmalignant monoclonal gammopathy. BMC Nephrol. 2016. 17. 17. 1-5.
46. Sainz-Prestel V., Hernandez-Perez J., Rojas-Rivera J., Milicua-Munoz J.М., Edigo J., Ortiz A. Rituximab-associated interstitial lung disease in fibrillary glomerulonephritis. Clin. Kidney J. 2013. 6. 510-2.
47. Cheung C.Y., Chan A.О.К., Chan G.P.Т., Iu H.Y.Р., Shek C.С., Chau K.F. Long-term of kidney transplantation in a patient with coexisting lipoprotein glomerulopathy and fibrillary glomerulonephritis. Clin. Kidney J. 2014. 7. 396-8.
48. Sekulic M., Nasr S.Н., Grande J.Р., Cornell L.D. Histologic regression of fibrillary glomerulonephritis: the first report of biopsy-proven spontaneous resolution of disease. Clin. Kidney J. 2017. 10 (6). 738-41.
49. Maroz N., Reuben S., Nadasdy T. Treatment of fibrillary glomerulonephritis with use of repository corticotropin injections. Clin. Kidney J. 2018. 11(6). 788-90.
50. Cantillo J.D.J., Lopez R.D.Р., Andrade R.E. Glomerular deposition disease, regarding a case of fibrillary glomerulonephritis. Biomed. 2009. 29. 539-46.
51. Yumura W., Nitta K., Horita S., Ozu H., Honda K., Nihei H. Nephrotic syndrome associated with fibrillary deposits in the glomeruli. Intern. Med. 1995. 34. 46-50.
52. Suzuki S., Konta T., Koizumi R., Nishida W., Abiko H., Kubota I. Fibrillary glomerulonephritis with hypocomplementemia. Intern. Med. 2003. 42. 719-22.
53. Sundaram S., Mainali R., Norfolk E.R., Shaw IV J.H., Zhang P.L. Fibrillary glomerulopathy secondary to light chain deposition disease in a patient with monoclonal gammopathy. Ann. Clin. Lab. Sci. 2007. 37 (4). 370-4.
54. Sehgal R., Sajjad S.M., Thapa J.K. Fibrillary glomerulonephritis in primary sjogren’s syndrome: A rare cause of renal failure. Clin. Med. Res. 2017. 15(3–4). 100-5.
55. Chaudhary A., Gyamlani G., Coosey N.L., Walker P.D., Wall B.M. Successful use of rituximab in fibrillary glomerulopathy. Ren. Fail. 2014. 36 (7). 1151-4.
56. Dussol B., Kaplanski G., Daniel L., Brunet P., Pellissier J.F., Berland Y. Simultaneous occurrence of fibrillary glomerulopathy and AL amyloid. Nephrol. Dial. Transplant. 1998. 13. 2630-2.
57. Ichikawa H., Ikeda S., Hashimoto M., Nagake Y., Hironaka K., Shikata K. et al. Fibrillary glomerulonephritis in a patient with familial sensorineural deafness. Nephrology. 1997. 3. 381-4.
58. Coroneos E., Truong L., Olivero J. Fibrillary glomerulonephritis associated with hepatitis C viral infection. Am. J. kidney Dis. 1997. 29 (1). 132-5.
59. Ray S., Rouse K., Appis A., Novak R., Haller N.A. Fibrillary glomerulonephritis with hepatitis C viral infection and hypocomplementemia. Ren. Fail. 2008. 30. 759-62.
60. Kim H.J., Kang S.W., Park S.J., Kim T.Н., Kang M.S., Kim Y.H. Fibrillary glomerulonephritis associated with Behcet’ Syndrome. Ren. Fail. 2012. 34(5). 637-9.
61. Soma J., Sato K., Nakaya I., Yahata M., Sakuma T., Sato H. Systemic non-amyloiditic fibril deposition disease: a probable variant form of fibrillary glomerulonephritis. Clin. Nephrol. 2011. 75 (1). 74-9.
62. Asakawa T., Asou M., Hara S., Ehara T., Araki M. Fibrillary glomerulopathy with high level of myeloperoxidase — ANCA: A case report. Case Rep. Nephrol. 2020. 2020. Article ID 6343521.
63. Gonzalez-Cabrera F., Henriquez-Palop F., Ramirez-Puga A. et al. The occurrence or fibrillary glomerulonephritis in patients with diabetes mellitus may not be coincidental: A report of four cases. Case Rep. Med. 2013. 2013. Article ID 935172.
64. Tsui C., Dokouhaki P., Prasad B. Fibrillary glomerulonephritis with crescentric and necrotizing glomerulonephritis and concurrent thrombotic microangiopathy. Case Rep. Nephrol. Dial. 2018. 8. 182-91.
65. Adey D.В., Macpherson B.R., Groggle G.C. Glomerulonephritis with associated hypocomplementemia and crescents: An unusual case of fibrillary glomerulonephritis. J. Am. Soc. Nephrol. 1995. 6. 171-6.
66. Rostagno A., Vidal R., Kumar A., Chuba J., Neiderman G., Gold L., et al. Fibrillary glomerulonephritis related to serum fibrillar immunoglobulin-fibronectin complexes. Am. J. Kidney Dis. 1996. 28(5). 676-84.
67. Hsu B.G., Chang C.H., Chiang S.S., Yang A.H. Fibrillary glomerulonephritis. Chinese Med. J. (Taipei). 2001. 64. 419-25.
68. Bircan Z., Toprak D., Kilicaslen I. et al. Factor H deficiency and fibrillary glomerulopathy. Nephrol. Dial. Transplant. 2004. 19. 727-30.
69. Cheung S.F., Yue T.Т., Lee K.C. Fibrillary glomerulopathy; report of a case and review of the literature. Hong Kong J. Nephrol. 1991. 1(1). 64-7.
70. Khorsan R., Ruan Q.N. Fibrillary glomerulonephritis. Proceed UCLA Health. 2021. 25. 1-2.
71. Nasr S.Н., Valeri A.М., Cornell L.D., Fidler M.Е., Sethi S., Leung N. et al. Fibrillary glomerulonephritis: A report of 66 cases from a single institution. Clin. J. Am. Soc. Nephrol. 2011. 6. 775-84.
72. Nasr S.Н., Dasari S., Lieske J.С., Benson L.М., Vanderboom P.М., Holtz-Hepplemann C.J. et al. Serum levels of DNAJB9 are elevated in fibrillary glomerulonephritis patients. Kidney Int. 2019. 95. 1269-72.
73. Andeen N.K., Smith K.D., Vasilescu E.R., Bata I. Fibrillary GN is associated with HLA-DR7 and HLA-B35 antigens. Kidney Int. Rep. 2020. 5. 1325-7.
74. Said S.М., Best Rocha A., Valeri A.М., Sandid M., Ray A.S., Fidler M.Е. et al. Characteristics of patients with coexisting with DNAjB9-associated fibrillary glomerulonephritis and IgA nephropathy. Clin. Kidney J. 2021. 6. 1681-90.
75. Payan Schober F., Jobson M.А., Poulton C.J., Singh H.K., Nickeleti V., Falki R.J. et al. Clinical features and outcomes of a racially diverse population with fibrillary glomerulonephritis. Am. J. Nephrol. 2017. 45. 248-56.
76. Marinaki S., Tsiakas S., Liapis G. et al. Clinicopathologic features and treatment outcomes of patients with fibrillary glomerulonephritis. Medicine. 2021. 100 (20). 1-6.
77. Dasari S., Alexander M.Р., Vrana J.А., Theis J.D., Mils J.R., Negron V. et al. DnaJ heat shock protein family B member 9 is a novel biomarker for fibrillary GN. J. Am. Soc. Nephrol. 2018. 29. 51-56.
/40.jpg)

/43.jpg)
/44.jpg)
/45.jpg)
/46.jpg)
/47.jpg)
/50.jpg)
/49.jpg)