Журнал «Медицина неотложных состояний» Том 20, №2, 2024
Вернуться к номеру
Епілептичний статус: сучасні погляди на класифікацію, типологію, методи діагностики та лікування протинападовими препаратами третього покоління (огляд)
Авторы: Мар’єнко Л.Б. (1), Дубенко А.Є. (2), Літовченко Т.А. (3)
(1) - Львівський національний медичний університет ім. Данила Галицького, м. Львів, Україна
(2) - ДУ «Інститут неврології, психіатрії та наркології НАМН України», ЛДЦЕ КНП ХОР «Обласна клінічна психіатрична лікарня № 3», Медичний центр «Нейрон», м. Харків, Україна
(3) - Харківський національний медичний університет, м. Харків, Україна
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
Епілептичний статус (ЕС) є невідкладною медичною ситуацією, пов’язаною з високою захворюваністю та смертністю. У рекомендаціях Міжнародної протиепілептичної ліги використовується поетапний підхід до терапії ЕС залежно від відповіді на лікування. Бензодіазепіни зазвичай використовуються як початкова терапія ЕС. Однак приблизно в 40 % випадків судомного ЕС при їх призначенні не спостерігається поліпшення, що свідчить про виникнення розгорнутого ЕС. Для його лікування застосовують внутрішньовенні протинападові препарати, такі як фосфенітоїн, вальпроат або леветирацетам. Але і ця терапія в 31–47 % може бути неефективною, що обумовлено розвитком рефрактерного або суперрефрактерного ЕС. Для боротьби з ними призначаються додаткові протинападові препарати.
Status epilepticus (SE) is a medical emergency associated with high morbidity and mortality. The guidelines of the International League Against Epilepsy use a stepwise approach to the treatment of SE depending on the response to treatment. Benzodiazepines are commonly used as initial therapy for SE. However, in approximately 40 % of cases of convulsive SE when benzodiazepines are prescribed, no improvement is observed, which indicates the occurrence of a refractory SE. For its treatment, intravenous anticonvulsants such as fosphenytoin, valproate or levetiracetam are used. But even this therapy can be ineffective in 31–47 % of cases, which is due to the development of refractory or super-refractory SE. To combat them, additional anti-seizure drugs are prescribed.
епілептичний статус; лікування; протинападові препарати
status epilepticus; treatment; anticonvulsants
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Willems L.M. Therapeutic Options for Patients with Refractory Status Epilepticus in Palliative Settings or with a Limitation of Life-Sustaining Therapies: A Systematic Review. CNS Drugs. 2020. 34. 801-826.
- Mitchel J., Adan G., Whitehead C., Musial G., Bennett R., Burness C. Status epilepticus guideline. NHS. May 2023. 3-38.
- Trinka E. et al. A definition and classification of status epilepticus — Report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia. Blackwell Publishing Inc. 2015. 56. 10. 1515-1523.
- Birrer K. et al. Management of Status Epilepticus in Adults. Evidence Based Medicine Guideline. Surgical Critical Care.net. 2022.
- Trinka E., Leitinger M. Management of Status Epilepticus, Refractory Status Epilepticus, and Super-refractory Status Epilepticus. Continuum (Minneap. Minn.). 2022. 28(2). 559-602.
- Brophy G.M., Bell R., Claasen J. et.al. Guidelines for the evaluation and management of status epilepticus. Neurocrit. Care. 2012.
- Glauser T., Shinnar S., Gloss D. et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline committee of the American Epilepsy Society. Epilepsia Curr. 2016. 16(1). 67-73.
- Claassen J., Goldstein J.N. Emergency neurologic life support: status epilepticus. Neurocrit. Care. 2017. 27 (Suppl. 1). 152-158.
- Kapur J., Elm J., Chamberlain J.M. et al. Randomized trial of three anticonvulsant medications for status epilepticus. N. Engl. J. Med. 2019. 381. 2103-2113.
- Grover E.H., Nazzal Y., Hirsch L.J. Treatment of convulsive status epilepticus. Curr. Treat. Opinions Neurol. 2016. 18. 11.
- Chakravarthi S., Goyal M.K., Modi M. et al. Levetiracetam versus phenytoin in management of status epilepticus. J. Clin. Neurosci. 2015. 22(6). 959-963.
- Yasiry Z., Shorvon S.D. The relative effectiveness of five antiepileptic drugs in treatment of benzodiazepineresistant convulsive status epilepticus: a meta-analysis of published studies. Seizure. 2014. 23. 167-174.
- Doty P., Hebert D., Mathy F.X. et al. Development of laco–samide for the treatment of partial-onset seizures. Ann. N. Y. Acad. Sci. 2013. 1291. 56-68.
- Höfler J., Trinka E. Lacosamide as a new treatment option in status epilepticus. Epilepsia. 2013. 54. 393-404.
- Miro J., Toledo M., Santamarina E. et al. Efficacy of intravenous lacosamide as an add-on treatment in refractory status epilepticus: a multicentric prospective study. Seizure. 2013. 22. 77-79.
- Rosenow F. The epidemiology of status epilepticus. Colloquium on Status epilepticus. Platform presentations abstracts. London. 2007. 59-60.
- Logroscino G., Hesdorffer D.C., Cascino G. Mortality after a first episode of status epilepticus in the United States and Europe. Epilepsia. 2005. 46. Suppl. 11. 46-48.
- Kortland L.M., Alfter A., Bahr O. et al. Costs and cost-driving factors for acute treatment of adults with status epilepticus: a multicenter cohort study from Germany. Epilepsia. 2016. 57. 2056-2066.
- Kortland L.M., Knake S., Rosenow F. et al. Cost of status epilepticus: a systematic review. Seizure. 2015. 24. 17-20.
- Ferlisi M., Shorvon S. The outcome of therapies in refractory and super-refractory convulsive status epilepticus and recommendations for therapy. Brain. 2012. 135. 2314-2328.
- Shorvon S., Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011. 134. 2802-2818.
- Perucca E. What is the promise of new antiepileptic drugs in status epilepticus? Focus on brivaracetam, carisbamate, lacosamide, NS1209, and topiramate. Epilepsia. 2009. 50 (Suppl. 12). 49-50.
- Glauser T., Ben-Menachem E., Bourgeois B. et al. Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia. 2013. 54. 551-563.
- Hoshiyama E., Kumasawa J., Uchida M. et al. Phenytoin versus other antiepileptic drugs as treatments for status epilepticus in adults: a systematic review and meta-analysis. Acute Med. Surg. 2022. 9. e717.
- Feng Y., Chen Y., Jia Y. et al. Efficacy and safety of levetiracetam versus fosphenytoin for second-line treatment of epilepticus: a meta-analysis of latest randomized controlled trials. Seizure. 2021. 91. 339-345.
- Santamarina E., Toledo M., Sueiras M. et al. Usefulness of intravenous lacosamide in status epilepticus. J. Neurol. 2013. 260. 3122-3128.
- Kellinghaus C., Berning S., Stogbauer F. Intravenous laco–samide or phenytoin for treatment of refractory status epilepticus. Acta Neurol. Scand. 2014. 129. 294-299.
- Strzelczyk A., Zöllner J.F., Willems L.M., Paule J.E., Schubert-Bast S., Rosenow F., Bauer S. Lacosamide in status epilepticus: Systematic review of current evidence. Epilepsia. 2017. 58(6). 933-950.
- Garcés M., Villanueva V., Mauri J.A. et al. Factors influencing response to intravenous lacosamide in emergency situations: LACO-IV study. Epilepsy Behav. 2014. 36. 144-152.
- Rüegg S. Nonconvulsive Status Epilepticus in Adults: Types, Pathophysiology, Epidemiology, Etiology, and Diagnosis. Neurology International. 2017. 1. E189-E203.
- Нunt D.L., Castillo P.E. Synaptic plasticity of NMDA receptros: Mechanisms and functional implications. Curr. Opin. Neurobiol. 2012. 22. 496-508
- Naylor D.E., Liu H., Niquet J. et al. Rapid surface accumulation of NMDA receptors increases glutamatergic excitation during status epilepticus. Neurobiol. Dis. 2013. 54. 225-238.
- Holzer F.J., Seeck M., Korff C.M. Autoimmunity and inflammation in status epilepticus: from concepts to therapies. Expert Rev. Neurother. 2014. 14. 1181-1202.
- Vezzani A., Dingledine R., Rossetti A.O. Immunity and inflammation in status epilepticus and its sequelae possibilities for therapeutic application. Expert Rev. Neurother. 2015. 15. 1081-1092.
- Fabene P.F., Navarro Mora G., Martinello M. et al. A role for leukocyte-endothelial adhesion mechanisms in epilepsy. Nat. Med. 2008. 14. 1377-1383.
- Henshall D.C. MicroRNAs in the pathophysiology and treatment of status epilepticus. Front. Mol. Neurosci. 2013. 6. 37.
- Worrell G.A., Cranstoun S.D., Echauz J. et al. Evidence of self-organized criticality in human epileptic hippocampus. Neuroreport. 2002. 13. 2017-2021.
- Lado F.A., Moshé S.L. How do seizures stop? Epilepsia. 2008. 49. 1651-1664.
- Treiman D.M., Walton N.Y., Kendrick C. A progressive sequence of electroencephalographic changes during generalized convulsive status epilepticus. Epilepsy Res. 1990. 5. 49-60.
- van der Lende M., Surges R., Sander J.W. et al. Cardiac arrhythmias during after epileptic seizures. J. Neurol. Neurosurg. Psychiatry. 2016. 87. 69-74.
- Rai S., Drislane F.W. Treatment of Refractory and Super-refractory Status Epilepticus. Neurotherapeutics. 2018. 15. 697-712.
- Holtkamp M., Othman J., Buchheim K., Masuhr F., Schielke E., Meierkord H. A “Bmalignant” variant of status epilepticus. Arch. Neurol. 2005. 62. 1428-1431.
- Holtkamp M. The anaesthetic and intensive care of status epilepticus. Curr. Opin. Neurol. 2007. 20. 188-193.
- Shorvon S., Ferlisi M. The treatment of super-refractory status epilepticus: a critical review of available therapies and a clinical treatment protocol. Brain. 2011. 134. 2802-2818.
- Brophy G.M., Bell R., Claassen J., Alldredge B., Bleck T.P., Glauser T. et al.; Neurocritical Care Society Status Epilepticus Guideline Writing Committee. Guidelines for the evaluation and management of status epilepticus. Neurocrit. Care. 2012. 17. 3-23.
- Shorvon S., Baulac M., Cross H., Trinka E., Walker M. TaskForce on Status Epilepticus of the ILAE Commission for European Affairs The drug treatment of status epilepticus in Europe: consensus document from a workshop at the first London Colloquium on Status Epilepticus. Epilepsia. 2008. 49. 1277-1285.
- Kantanen A.M., Reinikainen M., Parviainen I., Ruokonen E., Ala Peijari M., Bäcklund T. et al. Incidence and mortality of super-refractory status epilepticus in adults. Epilepsy Behav. 2015. 49. 131-134.
- Sutter R., Dittrich T., Semmlack S., Rüegg S., Marsch S., Kaplan P.W. Acute systemic complications of convulsive status epilepticus — a systematic review. Crit. Care Med. 2018. 46. 138-145.
- Devinsky O., Vezzani A., Najjar S., DeLanerolle N.C., Rogawski M.A. Glia and epilepsy: excitability and inflammation. Trends Neurosci. 2013. 36. 174-184.
- Cianfoni A., Caulo M., Cerase A., Della Marca G., Falcone C., Di Lella G.M. et al. Seizure induced brain lesions: a wide spectrum of variably reversible MRI abnormalities. Eur. J. Radiol. 2013. 82. 1964-1972.
- Pohlmann-Eden B., Gass A., Peters C.A., Wennberg R., Bluemcke I. Evolution of MRI changes and development of bilateral hippocampal sclerosis during long lasting generalised status epilepticus. J. Neurol. Neurosurg. Psychiatry. 2004. 75. 898-900.
- Cole A.J. Status epilepticus and periictal imaging. Epilepsia. 2004. 45 (Suppl. 4). 72-77.
- Alvarez V., Drislane F.W. Is favorable outcome possible after prolonged refractory status epilepticus? J. Clin. Neurophysiol. 2016. 33. 32-41.
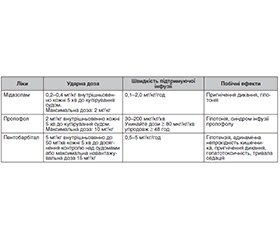
- Claassen J., Hirsch L.J., Emerson R.G., Mayer S.A. Treatment of refractory status epilepticus with pentobarbital, propofol, or midazolam: a systematic review. Epilepsia. 2002. 43. 146.
- Ferlisi M., Hocker S., Grade M., Trinka E., Shorvon S., of the StEp IS Preliminary results of the global audit of treatment of refractory status epilepticus. Epilepsy Behav. 2015. 49. 318-324.
- Herman S.T., Abend N.S., Bleck T.P., Chapman K.E., Drislane F.W., Emerson R.G. et al. Consensus statement on continuous EEG in critically ill adults and children, part I: indications. J. Clin. Neurophysiol. 2015. 32. 87-95.
- Rossetti A.O., Milligan T.A., Vulliémoz S., Michaelides C., Bertschi M., Lee J.W. A randomized trial for the treatment in refractory status epilepticus. Neurocrit. Care. 2011. 14. 4-10.
- Claassen J., Hirsch L.J., Emerson R.G., Bates J.E., Thompson T.B., Mayer S.A. Continuous EEG monitoring and midazolam infusion for refractory nonconvulsive status epilepticus. Neurology. 2001. 57. 1036-1042.
- Brenner R.P. Is it status? Epilepsia. 2002. 43 (Suppl. 3). 103-113.
- Hocker S., Tatum W.O., LaRoche S., Freeman W.D. Refractory and super-refractory status epilepticus — an update. Curr. Neurol. Neurosci. Rep. 2014. 14. 452.
- Sutter R., Marsch S., Fuhr P., Kaplan P.W., Rüegg S. Anesthetic drugs in status epilepticus: risk or rescue? A 6-year cohort study. Neurology. 2014. 82. 656-664.
- Marchi N.A., Novy J., Faouzi M., Stähli C., Burnand B., Rossetti A.O. Status epilepticus: impact of therapeutic coma on outcome. Crit. Care Med. 2015. 43. 1003-1009.
- Wheless J.W. Acute management of seizures in the syndromes of idiopathic generalized epilepsies. Epilepsia. 2003. 44 (Suppl. 2). 22-26.
- Misra U.K., Kalita J., Maurya P.K. Levetiracetam versus lorazepam in status epilepticus: a randomized, open labeled pilot study. J. Neurol. 2012. 259. 645-648.
- Holtkamp M. Pharmacotherapy for refractory and super-refractory status epilepticus in adults. Drugs. 2018. 78. 307-326.
- Besha A., Adamu Y., Mulugeta H., Zemedkun A., Destaw B. Evidence-based guideline on management of status epilepticus in adult intensive care unit in resource-limited settings: a review article. Ann. Med. Surg. (Lond.). 2023 Apr 17. 85(6). 2714-2720.