Международный эндокринологический журнал Том 20, №3, 2024
Вернуться к номеру
Патогенетична основа лікування метформіном ендотеліальної дисфункції у пацієнтів з цукровим діабетом (огляд літератури та власних даних)
Авторы: Соколова А.М. (1), Пушкарьов В.В. (2), Соколова Л.К. (2), Пушкарьов В.М. (2), Тронько М.Д. (2)
(1) - Національний медичний університет імені О.О. Богомольця, м. Київ, Україна
(2) - ДУ «Інститут ендокринології та обміну речовин імені В.П. Комісаренка НАМН України», м. Київ, Україна
Рубрики: Эндокринология
Разделы: Справочник специалиста
Версия для печати
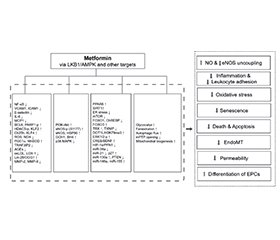
Серцево-судинні розлади є однією з головних причин смертності та захворюваності в усьому світі, і ймовірність зростає з додаванням таких факторів ризику, як малорухливий спосіб життя, діабет, ожиріння, гіперліпідемія та гіпертонія. Підвищення рівня цукру в крові може призвести до окиснювального стресу, дисліпідемії та ендотеліальної дисфункції, що завершується підвищеним серцево-судинним ризиком. Гіперглікемія шкідливо впливає на серцево-судинну систему, вона є причиною мікро- та макросудинних захворювань. Шкідливі біохімічні механізми гіперглікемії пов’язані з явищем резистентності до інсуліну. Метформін (МФ) послаблює інсулінорезистентність і, отже, здійснює антигіперглікемічний та інсулінознижувальний ефект у пацієнтів з діабетом 2-го типу. МФ так само, як гіполіпідемічні статини, також здійснює додатковий сприятливий плейотропний, протизапальний та антиоксидантний вплив на судинну систему, крім його гіполіпідемічної і антигіперглікемічної дії. Основним є вплив МФ на ендотеліальну дисфункцію, оскільки цілісність ендотелію є критичним і довгостроковим фактором здоров’я судин, а отже, виникнення серцево-судинних захворювань. МФ має дуже просту хімічну структуру. Проста структура означає, що розробка нових агентів з подібними або кращими властивостями та механізмами дії малоймовірна, тому у майбутньому варто розраховувати на використання даних фармакокінетики, фармакодинаміки та терапевтичного таргетування для розкриття повного терапевтичного потенціалу МФ. Цей підхід нещодавно було продемонстровано на прикладі препарату МФ з уповільненим вивільненням, який діє у дистальному відділі кишечника та виявляє кишкову гормонозалежну антигіперглікемічну дію. Практично не існує прихованих небажаних ефектів для МФ, тому він має потенціал для забезпечення ефективного та безпечного лікування гіперглікемії у майбутньому, особливо через сприятливий вплив на серцево-судинні захворювання, включно з ендотеліальною дисфункцією і атеросклерозом.
Cardiovascular disorders are one of the leading causes of mortality and morbidity worldwide, and their likelihood increases with the addition of risk factors such as sedentary lifestyle, diabetes, obesity, hyperlipidemia, and hypertension. Elevated blood sugar levels can lead to oxidative stress, dyslipidemia, and endothelial dysfunction, culminating in increased cardiovascular risk. Hyperglycemia adversely affects the cardiovascular system, it is a cause of micro- and macrovascular diseases. Harmful biochemical mechanisms of hyperglycemia are associated with the phenomenon of insulin resistance. Metformin (MF) reduces insulin resistance and, therefore, exerts an antihyperglycemic and insulin-lowering effect in patients with type 2 diabetes. MF, like hypolipidemic statins, also has an additional beneficial pleiotropic, anti-inflammatory and antioxidant effect on the vascular system, in addition to its hypolipidemic and antihyperglycemic effects. Primary is the effect of MF on endothelial dysfunction, as endothelial integrity is a critical long-term determinant of vascular health and, therefore, the occurrence of cardiovascular disease. MF has a very simple chemical structure. The simple structure means that the development of new agents with similar or better properties and mechanisms of action is unlikely, so future use of pharmacokinetic, pharmacodynamic and therapeutic targeting data should be expected to unlock the full therapeutic potential of MF. This approach has recently been demonstrated using a sustained-release MF drug that acts in the distal intestine and exhibits intestinal hormone-dependent antihyperglycemic effect. There are virtually no hidden adverse effects for MF, so it has the potential to provide an effective and safe treatment for hyperglycemia in the future, particularly through its beneficial effects on cardiovascular diseases, including endothelial dysfunction and atherosclerosis.
ендотеліальна дисфункція; атеросклероз; цукровий діабет; метформін; огляд
endothelial dysfunction; atherosclerosis; diabetes; metformin; review
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Dutta S, Shah RB, Singhal S, Dutta SB, Bansal S, Sinha S, et al. Metformin: A Review of Potential Mechanism and Therapeutic Utility Beyond Diabetes. Drug Des Devel Ther. 2023 Jun 26;17:1907-1932. doi: 10.2147/DDDT.S409373.
- Libby P. Inflammation and the pathogenesis of atherosclerosis. Vascul Pharmacol. 2024;154:107255. doi: 10.1016/j.vph.2023.107255.
- Tokarek J, Budny E, Saar M, Stańczak K, Wojtanowska E, Młynarska E, et al. Molecular Processes Involved in the Shared Pathways between Cardiovascular Diseases and Diabetes. Biomedicines. 2023 Sep 23;11(10):2611. doi: 10.3390/biomedicines11102611.
- Triggle CR, Ding H, Marei I, Anderson TJ, Hollenberg MD. Why the endothelium? The endothelium as a target to reduce diabetes-associated vascular disease. Can. J. Physiol. Pharmacol. 2020;98(7):415-430. doi.org/10.1139/cjpp-2019-0677.
- Triggle CR, Marei I, Ye K, Ding H, Anderson TJ, Hollenberg MD, et al. Repurposing Metformin for Vascular Disease. Curr Med Chem. 2023;30(35):3955-3978. doi: 10.2174/0929867329666220729154615.
- Muscoli S, Ifrim M, Russo M, Candido F, Sanseviero A, Milite M, et al. Current Options and Future Perspectives in the Treatment of Dyslipidemia. J Clin Med. 2022 Aug 12;11(16):4716. doi: 10.3390/jcm11164716.
- Poznyak AV, Litvinova L, Poggio P, Moschetta D, Sukhorukov VN, Orekhov AN. From Diabetes to Atherosclerosis: Potential of Metformin for Management of Cardiovascular Disease. Int J Mol Sci. 2022 Aug 27;23(17):9738. doi: 10.3390/ijms23179738.
- Javadipour M, Rezaei M, Keshtzar E, Khodayar MJ. Metformin in contrast to berberine reversed arsenic-induced oxidative stress in mitochondria from rat pancreas probably via Sirt3-dependent pathway. J Biochem Mol Toxicol. 2019 Sep;33(9):e22368. doi: 10.1002/jbt.22368.
- Serhiyenko V, Serhiyenko A. Diabetes mellitus and congestive heart failure. International Journal оf Endocrinology (Ukraine). 2022;18(1):57-69. https://doi.org/10.22141/2224-0721.18.1.2022.1146.
- Cen J, Sargsyan E, Forslund A, Bergsten P. Mechanisms of Beneficial Effects of Metformin on Fatty Acid-Treated Human Islets. J. Mol. Endocrinol. 2018 Oct 1;61(3):91-99. doi: 10.1530/JME-17-0304.
- Roxo DF, Arcaro CA, Gutierres VO, Costa MC, Oliveira JO, Lima TFO, et al. Curcumin Combined with Metformin Decreases Glycemia and Dyslipidemia, and Increases Paraoxonase Activity in Diabetic Rats. Diabetol. Metab. Syndr. 2019 Apr 30:11:33. doi: 10.1186/s13098-019-0431-0.
- Andreadi A, Muscoli S, Tajmir R, Meloni M, Muscoli C, Ilari S, et al. Recent Pharmacological Options in Type 2 Diabetes and Synergic Mechanism in Cardiovascular Disease. Int J Mol Sci. 2023 Jan 13;24(2):1646. doi: 10.3390/ijms24021646.
- Zhao LP, Sheng XY, Zhou S, Yang T, Ma LY, Zhou Y et al. Metformin versus insulin for gestational diabetes mellitus: A meta-ana–lysis. British Journal of Clinical Pharmacology 2015 Nov;80(5):1224-34. doi: 10.1111/bcp.12672.
- Defronzo RA, Buse JB, Kim T, Burns C, Skare S, Baron A, et al. Once-daily delayed-release metformin lowers plasma glucose and enhances fasting and postprandial GLP-1 and PYY: Results from two randomised trials. Diabetologia. 2016 Aug;59(8):1645-54. doi: 10.1007/s00125-016-3992-6.
- Vatseba TS, Sokolova LK, Pushkarev VM, Kovzun OI, Guda BB, Pushkarev VV, Tronko MD et al. Activation of the PI3K/AKT/MTOR/P70S6K1 signaling cascade in peripheral blood mononuclear cells in patients with type 2 diabetes. Ukr. Biochem. J. 2020;92(6):113-118. doi: https://doi.org/10.15407/ubj92.06.113.
- Koval SM, Yushko KO, Snihurska IO, Starchenko TG, Pankiv VI, Lytvynova OM, Mysnychenko OV. Relations of angiotensin-(1-7) with hemodynamic and cardiac structural and functional parameters in patients with hypertension and type 2 diabetes. Arterial Hypertension. 2019;23(3):183-189. DOI: 10.5603/AH.a2019.0012.
- Nafisa A, Gray SG, Cao Y, Wang T, Xu S, Wattoo FH, et al. Endothelial function and dysfunction: Impact of metformin. Pharmacol Ther. 2018 Dec;192:150-162. doi: 10.1016/j.pharmthera. 2018.07.007.
- Vatseba T, Sokolova L, Koshel N. Assessment of the prognostic cancer risk in patients with type 2 diabetes mellitus. International Journal оf Endocrinology (Ukraine). 2021:17(1):86-91. https://doi.org/10.22141/2224-0721.17.1.2021.226437.
- Sokolova LK, Pushkarev VM, Belchina YuB, Pushkarev VV, Tronko ND. Activity of adenosine monophosphate-activated protein kinase in lymphocytes under the action of hypoglycemic drugs. Dopov Nats Akad Nauk Ukr. 2017;(6):96-100. doi: 10.24026/1818- 1384.2(58).2017.105627.
- Sokolova LK, Pushkarev VM, BelchynaYuB, Pushkarev VV, Gonchar IV, Tronko MD. AMPK activity in lymphocytes of patients with diabetes under the influence of hypoglycemic drugs. Clinical Endocrinology and Endocrine Surgery. 2017;(2):82-90. (Ukrainian). doi: 10.24026/1818-1384.2(58).2017.105627.
- Sokolova L, Belchina Y, Pushkarev V, Cherviakova S, Vatseba T, Kovzun O, Pushkarev V, Tronko M. The effect of metformin treatment on the level of GLP-1, NT-proBNP and endothelin-1 in patients with type 2 diabetes mellitus. International Journal оf Endocrinology (Ukraine). 2020:16(8):616-621. https://doi.org/10.22141/2224-0721.16.8.2020.222882.
- Pushkarev VV, Sokolova LK, Pushkarev VM, Belchina YuB, Vatseba TS, Tronko ND. Effect of combined treatment with insulin and other hypoglycemic drugs on 5’AMP-activated protein kinase activity in lymphocytes in patients with diabetes mellitus. Problemy endokrynnoyi patolohiyi. 2019;(3):74-82. doi: 10.21856/j-PEP.2019.3.10.
- Sourris KC, Lyons JG, de Courten MP, et al. c-Jun NH2-terminal kinase activity in subcutaneous adipose tissue but not nuclear factor-kappaB activity in peripheral blood mononuclear cells is an independent determinant of insulin resistance in healthy individuals. Diabetes. 2009 Jun;58(6):1259-65. doi: 10.2337/db08-1725.
- Motta BP, Pinheiro CG, Figueiredo ID, Cardoso FN, Oli–veira JO, Machado RTA, et al. Combined Effects of Lycopene and Metformin on Decreasing Oxidative Stress by Triggering Endogenous Antioxidant Defenses in Diet-Induced Obese Mice. Molecules. 2022 Dec 3;27(23):8503. doi: 10.3390/molecules27238503.
- Hamidi Shishavan M, Henning RH, van Buiten A, Goris M, Deelman L, et al. Metformin improves endothelial function and reduces blood pressure in diabetic spontaneously hypertensive rats independent from glycemia control: comparison to vildagliptin. Scientific Reports Sci Rep. 2017 Sep 8;7(1):10975. doi: 10.1038/s41598-017-11430-7.
- An H, Wei R, Ke J, Yang J, Liu Y, Wang X. et al. Metformin attenuates fluctuating glucose-induced endothelial dysfunction through enhancing GTPCH1- mediated eNOS recoupling and inhibiting NADPH oxidase. J Diabetes Complications. 2016 Aug;30(6):1017-24. doi: 10.1016/j.jdiacomp.2016.04.018.
- Zhang J, Cao M, Yang W, Sun F, Xu C, Yin L, et al. Inhibition of Glucose-6-phosphate dehydrogenase could enhance 1,4-benzoquinone-induced oxidative damage in K562 cells. Oxid Med Cell Longev. 2016:2016:3912515. doi: 10.1155/2016/3912515.
- Triggle CR, Ding H. Metformin is not just an antihyperglycaemic drug but also has protective effects on the vascular endothelium. Acta Physiol (Oxf). 2017 Jan;219(1):138-151. doi: 10.1111/apha.12644.
- He L, Wondisford FE. Metformin action: Concentrations matter. Cell Metab. 2015 Feb 3;21(2):159-162. doi: 10.1016/j.cmet.2015.01.003.
- Ke J, Liu Y, Yang J, Lu R, Tian Q, Hou W, et al. Synergistic effects of metformin with liraglutide against endothelial dysfunction through GLP-1 receptor and PKA signalling pathway. Sci Rep. 2017 Feb 1:7:41085. doi: 10.1038/srep41085.
- Zhang K, Yang W, Dai H, Deng Z. Cardiovascular risk following metformin treatment in patients with type 2 diabetes mellitus: results from meta-analysis. Diabetes Res Clin Pract. 2020;160:108001. doi: 10.1016/j.diabres.2020.108001.
- Han Y, Xie H, Liu Y, Gao P, Yang X, Shen Z. Effect of metformin on all-cause and cardiovascular mortality in patients with coronary artery diseases: a systematic review and an updated meta-analysis. Cardiovasc Diabetol. 2019;18(1):96. doi: 10.1186/s12933-019-0900-7.
- de Jager J, Kooy A, Schalkwijk C, van der Kolk J, Lehert P, Bets D, et al. Long-term effects of metformin on endothelial function in type 2 diabetes: Randomized Controlled Trial J Intern Med. 2014 Jan;275(1):59-70. doi: 10.1111/joim.12128.
- Heidarpour M, Mojarad M, Mazaheri-Tehrani S, Kachuei A, Najimi A, Shafie D, Rezvanian H. Comparative Effectiveness of Antidiabetic Drugs as an Additional Therapy to Metformin in Women with Polycystic Ovary Syndrome: A Systematic Review of Metabolic Approaches. Int J Endocrinol. 2024 Mar 11;2024:9900213. doi: 10.1155/2024/9900213. PMID: 38500709; PMCID: PMC10948218.
- Kaya MG, Yildirim S, Calapkorur B, Akpek M, Unluhizarci K, Kelestimur F. Metformin improves endothelial function and carotid intima media thickness in patients with PCOS. Randomized Controlled Trial Gynecol Endocrinol. 2015 May;31(5):401-5. doi: 10.3109/09513590.2015.1006188.
- Salvatore T, Pafundi PC, Galiero R, et al. Can metformin exert as an active drug on endothelial dysfunction in diabetic subjects? Biomedicines. 2020;9(1):3. doi: 10.3390/biomedicines9010003.
- Sutkowska E, Fortuna P, Kałuża B, Sutkowska K, Wiśniewski J, Prof AG. Metformin has no impact on nitric oxide production in patients with pre-diabetes. Biomed Pharmacother. 2021;140:111773. doi: 10.1016/j.biopha.2021.111773.
- An Y, Xu BT, Wan SR, Ma XM, Long Y, Xu Y, Jiang ZZ. The role of oxidative stress in diabetes mellitus-induced vascular endothelial dysfunction. Cardiovasc Diabetol. 2023 Sep 2;22(1):237. doi: 10.1186/s12933-023-01965-7.
- Hung CH, Chan SH, Chu PM, Lin HC, Tsai KL. Metformin regulates oxLDL-facilitated endothelial dysfunction by modulation of SIRT1 through repressing LOX-1-modulated oxidative signaling. Oncotarget. 2016 Mar 8;7(10):10773-87. doi: 10.18632/oncotarget.7387.
- Ding Y, Zhou Y, Ling P, Feng X, Luo S, Zheng X, et al. Metformin in cardiovascular diabetology: a focused review of its impact on endothelial function. Theranostics. 2021 Sep 9;11(19):9376-9396. doi: 10.7150/thno.64706.
- Kang L, Yi J, Lau CW, He L, Chen Q, Xu S, et al. AMPK-Dependent YAP Inhibition Mediates the Protective Effect of Metformin against Obesity-Associated Endothelial Dysfunction and Inflammation. Antioxidants (Basel). 2023 Aug 28;12(9):1681. doi: 10.3390/antiox12091681.
- Cheang WS, Tian XY, Wong WT, Lau CW, Lee SS, Chen ZY, et al. Metformin protects endothelial function in diet-induced obese mice by inhibition of endoplasmic reticulum stress through 5' adeno–sine monophosphate-activated protein kinase-peroxisome proliferator-activated receptor δ pathway. Arterioscler Thromb Vasc Biol. 2014 Apr;34(4):830-6. doi: 10.1161/ATVBAHA.113.3019.
- Pushkarev VV, Sokolova LK, Kovzun OI, Pushkarev VM, Tronko MD. The role of endoplasmic reticulum stress and NLRP3 inflammasomes in the development of atherosclerosis. Cytology and Genetics. 2021;55(4):331-9. doi: 10.3103/S0095452721040113.
- Kapadia P, Bikkina P, Landicho MA, Parekh S, Haas MJ, Mooradian AD. Effect of anti-hyperglycemic drugs on endoplasmic reticulum (ER) stress in human coronary artery endothelial cells. Eur J Pharmacol. 2021 Sep 15:907:174249. doi: 10.1016/j.ejphar.2021.174249.
- Venu VKP, Saifeddine M, Mihara K, Faiza M, Gorobets E, Flewelling AJ, et al. Metformin Prevents Hyperglycemia-Associated, Oxidative Stress-Induced Vascular Endothelial Dysfunction: Essential Role for the Orphan Nuclear Receptor Human Nuclear Receptor 4A1 (Nur77). Mol Pharmacol. 2021 Nov;100(5):428-455. doi: 10.1124/molpharm.120.000148.
- Sambe T, Mason RP, Dawoud H, Bhatt DL, Malinski T. Metformin treatment decreases nitroxidative stress, restores nitric oxide bioavailability and endothelial function beyond glucose control. Biomed Pharmacother. 2018 Feb:98:149-156. doi: 10.1016/j.biopha.2017.12.023.
- Tao L, Fan X, Sun J, Zhang Z. Metformin prevented high glucose-induced endothelial reactive oxygen species via OGG1 in an AMPKα-Lin-28 dependent pathway. Life Sci. 2021 Mar 1:268:119015. doi: 10.1016/j.lfs.2020.119015.
- Forzano I, Avvisato R, Varzideh F, Jankauskas SS, Cioppa A, Mone P, Salemme L, et al. L-Arginine in diabetes: clinical and preclinical evidence. Cardiovasc Diabetol. 2023 Apr 18;22(1):89. doi: 10.1186/s12933-023-01827-2. Erratum in: Cardiovasc Diabetol. 2023 May 18;22(1):117. PMID: 37072850; PMCID: PMC10114382.
- Yu JW, Deng YP, Han X, Ren GF, Cai J, Jiang GJ. Metformin improves the angiogenic functions of endothelial progenitor cells via activating AMPK/eNOS pathway in diabetic mice. Cardiovasc Diabetol. 2016 Jun 18;15:88. doi: 10.1186/s12933-016-0408-3.
- Kidokoro K, Satoh M, Channon KM, Yada T, Sasaki T, Kashihara N. Maintenance of endothelial guanosine triphosphate cyclohydrolase I ameliorates diabetic nephropathy. Journal Am Soc Nephrol. 2013 Jun;24(7):1139-50. doi: 10.1681/ASN.2012080783.
- Cheng L, Wang L, Guo M, He J, Deng Y, Liu J, et al. Clini–cally relevant high levels of human C-reactive protein induces endothelial dysfunction and hypertension by inhibiting the AMPK-eNOS axis. Clin Sci (Lond). 2020 Jul 17;134(13):1805-1819. doi: 10.1042/CS20200137.
- Avogaro A, Azzolina D, Gregori D, De Kreutzenberg S, Fadini GP, Mannucci E. The effect of GLP-1 receptor agonists on N-terminal pro-brain natriuretic peptide. A scoping review and metana–lysis. Int J Cardiol. 2022 Jun 15;357:123-127. doi: 10.1016/j.ijcard.2022.03.032. Epub 2022 Mar 16. PMID: 35306033.
- Inggriani MP, Musthafa A, Puspitawati I, Fachiroh J, Dewi FST, Hartopo AB. Increased endothelin-1 levels in coronary artery disease with diabetes mellitus in an Indonesian population. Can J Physiol Pharmacol. 2022 Dec 1;100(12):1097-1105. doi: 10.1139/cjpp-2022-0011. Epub 2022 Oct 28. PMID: 36305520.
- Detaille D, Guigas B, Chauvin C, Batandier C, Fontaine E, Wiernsperger N, et al. Metformin prevents high-glucose-induced endothelial cell death through a mitochondrial permeability transition-dependent process. Diabetes. 2005 Jul;54(7):2179-87. doi: 10.2337/diabetes.54.7.2179.
- Ye J, Li L, Wang M, Ma Q, Tian Y, Zhang Q, Liu J, et al. Diabetes Mellitus Promotes the Development of Atherosclerosis: The Role of NLRP3. Front Immunol. 2022 Jun 29;13:900254. doi: 10.3389/fimmu.2022.900254. PMID: 35844498; PMCID: PMC9277049.
- Agarwal SM, Panda R, Costa-Dookhan KA, MacKenzie NE, Treen QC, Caravaggio F, Hashim E, et al. Metformin for early comorbid glucose dysregulation and schizophrenia spectrum disorders: a pilot double-blind randomized clinical trial. Transl Psychiatry. 2021 Apr 14;11(1):219. doi: 10.1038/s41398-021-01338-2. PMID: 33854039; PMCID: PMC8046796.
- Laouirem S, Sannier A, Norkowski E, Cauchy F, Doblas S, Rautou PE, et al. Endothelial fatty liver binding protein 4: a new targetable mediator in hepatocellular carcinoma related to metabolic syndrome. Oncogene. 2019 Apr;38(16):3033-3046. doi: 10.1038/s41388-018-0597-1.
- Xu XX, Zhang SS, Lin HL, Lin Q, Shen LE, Ansong E, et al. Metformin promotes regeneration of the injured endometrium via inhibition of endoplasmic reticulum stress-induced apoptosis. Reprod Sci. 2019 Apr;26(4):560-568. doi: 10.1177/1933719118804424.
- Han X, Wang B, Sun Y, Huang J, Wang X, Ma W, et al. Metformin modulates high glucose-incubated human umbilical vein endothelial cells proliferation and apoptosis through AMPK/CREB/BDNF pathway. Front Pharmacol. 2018 Nov 6:9:1266. doi: 10.3389/fphar.2018.01266.
- Bakhashab S, Ahmed F, Schulten HJ, Ahmed FW, Glanville M, Al-Qahtani MH, et al. Proangiogenic effect of metformin in endothelial cells is via upregulation of VEGFR1/2 and their signaling under hyperglycemia-hypoxia. Int J Mol Sci. 2018 Jan 19;19(1):293. doi: 10.3390/ijms19010293.
- Hunt NJ, Lockwood GP, Kang SWS, Pulpitel T, Clark X, Mao H, et al. The effects of metformin on age-related changes in the liver sinusoidal endothelial cell. J Gerontol A Biol Sci Med Sci. 2020 Jan 20;75(2):278-285. doi: 10.1093/gerona/glz153.
- Zhang E, Guo Q, Gao H, Xu R, Teng S, Wu Y. Metformin and resveratrol inhibited high glucose-induced metabolic memory of endothelial senescence through SIRT1/p300/p53/p21 pathway. PLoS One. 2015 Dec 2;10(12):e0143814. doi: 10.1371/journal.pone.0143814.
- Lu Y, Yuan T, Min X, Yuan Z, Cai Z. AMPK: potential therapeutic target for vascular calcification. Front Cardiovasc Med. 2021 May 11:8:670222. doi: 10.3389/fcvm.2021.670222.
- Mohammed I, Hollenberg MD, Ding H, Triggle CR. A cri–tical review of the evidence that metformin is a putative anti-aging drug that enhances healthspan and extends lifespan. Front. Endocrinol. (Lausanne). 2021;12:718942. doi.org/10.3389/fendo.2021.718942.
- Yang Y, Dong R, Hu D, Chen Z, Fu M, Wang DW, Tu, L. Liver kinase B1/AMP-activated protein kinase pathway activation attenuated the progression of endotoxemia in the diabetic mice. Cell Physiol Biochem. 2017;42(2):761-779. doi: 10.1159/000478068.
- Ding H, Chen B, Lu Q, Wang J. Profilin-1 mediates microvascular endothelial dysfunction in diabetic retinopathy through HIF-1α-dependent pathway. Int J Clin Exp Pathol. 2018;11(3): 1247-55.
- Uddin MA, Akhter MS, Kubra KT, Siejka A, Barabutis N. Metformin in acute respiratory distress syndrome: an opinion. Exp Gerontol. 2021;145:111197. doi: 10.1016/j.exger.2020.11119.
- Asgharzadeh F, Barneh F, Fakhraie M, Adel Barkhordar SL, Shabani M, Soleimani A, et al. Metformin inhibits polyphosphate-induced hyper-permeability and inflammation. Int Immunopharmacol. 2021;99:107937. doi: 10.1016/j.intimp.2021.107937.
- Eelen G, de Zeeuw P, Treps L, Harjes U, Wong BW, Carme–liet P. Endothelial cell metabolism. Physiol Rev. 2018;98(1):3-58. doi: 10.1152/physrev.00001.2017.
- Andrade J, Shi C, Costa ASH, Choi J, Kim J, Doddaballapur A, et al. Control of endothelial quiescence by FOXO-regulated metabolites. Nat Cell Biol. 2021;23(4):413-23. doi: 10.1038/s41556-021-00637-6.
- Cabodevilla AG, Tang S, Lee S, Mullick AE, Aleman JO, Hussain MM, et al. Eruptive xanthoma model reveals endothelial cells internalize and metabolize chylomicrons, leading to extravascular triglyceride accumulation. J Clin Invest. 2021;131(12): e145800. doi: 10.1172/JCI145800.
- Kim HS, Ren G, Kim T, Bhatnagar S, Yang Q, Bahk YY, et al. Metformin reduces saturated fatty acid-induced lipid accumulation and inflammatory response by restoration of autophagic flux in endothelial cells. Sci Rep. 2020;10(1):13523. doi: 10.1038/s41598-020-70347-w.
- Samuel SM, Ghosh S, Majeed Y, Arunachalam G, Emara MM, Ding H, Triggle CR. Metformin represses glucose starvation induced autophagic response in microvascular endothelial cells and promotes cell death. Biochem Pharmacol. 2017 May 15:132:118-132. doi: 10.1016/j.bcp.2017.03.001.
- Dri E, Lampas E, Lazaros G, Lazarou E, Theofilis P, Tsioufis C, Tousoulis D. Inflammatory Mediators of Endothelial Dysfunction. Life (Basel). 2023 Jun 20;13(6):1420. doi: 10.3390/life13061420.
- Tian R, Li R, Liu Y, Liu J, Pan T, Zhang R, et al. Metformin ameliorates endotoxemia-induced endothelial pro-inflammatory responses via AMPK-dependent mediation of HDAC5 and KLF2. Biochim Biophys Acta Mol Basis Dis. 2019;1865(6):1701-12. doi: 10.1016/j.bbadis.2019.04.009.
- Han J, Li Y, Liu X, Zhou T, Sun H, Edwards P, et al. Metformin suppresses retinal angiogenesis and inflammation in vitro and in vivo. PLoS One. 2018b;13(3):e0193031. doi: 10.1371/journal.pone.0193031.
- Ahmadi A, Panahi Y, Johnston TP, Sahebkar A. Antidiabetic drugs and oxidized low-density lipoprotein: A review of anti-atherosclerotic mechanisms. Pharmacol Res. 2021;172:105819. doi: 10.1016/j.phrs.2021.105819.
- Wu H, Feng K, Zhang C, Zhang H, Zhang J, Hua Y, et al. Metformin attenuates atherosclerosis and plaque vulnerability by upregulating KLF2-mediated autophagy in apoE(-/-) mice. Biochem Biophys Res Commun. 2021;557:334-41. doi: 10.1016/j.bbrc.2021.04.029.
- Sundararajan S, Jayachandran I, Pandey GK, Venkatesan S, Rajagopal A, Gokulakrishnan K, et al. Metformin Reduces the Progression of Atherogenesis by Regulating the Sestrin2-mTOR Pathway in Obese and Diabetic Rats. J Lipid Atheroscler. 2023 Sep;12(3):290-306. doi: 10.12997/jla.2023.12.3.290.
- Valente AJ, Irimpen AM, Siebenlist U, Chandrasekar B. OxLDL induces endothelial dysfunction and death via TRAF3IP2: inhibition by HDL3 and AMPK activators. Free Radic Biol Med. 2014 May;70:117-28. doi: 10.1016/j.freeradbiomed.2014.02.014. Epub 2014 Feb 20. PMID: 24561578; PMCID: PMC4006317.
- Bridgeman SC, Ellison GC, Melton PE, Newsholme P, Mamotte CDS. Epigenetic effects of metformin: From molecular mechanisms to clinical implications. Diabetes Obes Metab. 2018 Jul;20(7):1553-1562. doi: 10.1111/dom.13262. Epub 2018 Mar 22. PMID: 29457866.
- Karnewar S, Neeli PK, Panuganti D, Kotagiri S, Mallappa S, Jain N, Jerald MK, Kotamraju S. Metformin regulates mitochondrial biogenesis and senescence through AMPK mediated H3K79 methylation: Relevance in age-associated vascular dysfunction. Biochim Biophys Acta Mol Basis Dis. 2018 Apr;1864(4 Pt A):1115-1128. doi: 10.1016/j.bbadis.2018.01.018. Epub 2018 Jan 31. PMID: 29366775.
- Chen YC, Kuo CH, Tsai YM, Lin YC, Hsiao HP, Chen B, et al. Suppressive effects of metformin on T-helper 1-related chemokines expression in the human monocytic leukemia cell line THP-1. Endocr Res. 2018 Nov;43(4):228-234. doi: 10.1080/07435800.2018.1460605.
- Tang G, Guo J, Zhu Y, Huang Z, Liu T, Cai J, Wang, Z. Metformin inhibits ovarian cancer via decreasing H3K27 trimethylation. Int J Oncol. 2018 Jun;52(6):1899-1911. doi: 10.3892/ijo.2018.4343.
- Xu S, Xu Y, Yin M, Zhang S, Liu P, Koroleva M, et al. Flow-dependent epigenetic regulation of IGFBP5 expression by H3K27me3 contributes to endothelial anti-inflammatory effects. Theranostics. 2018 Apr 30;8(11):3007-3021. doi: 10.7150/thno.21966.
- Arunachalam G, Lakshmanan AP, Samuel SM, Triggle CR, Ding H. Molecular interplay between microRNA-34a and sirtuin1 in hyperglycemia-mediated impaired angiogenesis in endothelial cells: effects of metformin. J Pharmacol Exp Ther. 2016;356(2):314-23. doi: 10.1124/jpet.115.226894.
- Ni HZ, Liu Z, Sun LL, Zhou M, Liu C, Li WD, et al. Metformin inhibits angiogenesis of endothelial progenitor cells via miR-221-mediated p27 expression and autophagy. Future Med Chem. 2019;11(17):2263-72. doi: 10.4155/fmc-2019-0017.
- Gou L, Liu G, Ma R, Regmi A, Zeng T, Zheng J, et al. High fat-induced inflammation in vascular endothelium can be improved by Abelmoschus esculentus and metformin via increasing the expressions of miR-146a and miR-155. Nutr Metab (Lond). 2020;17:35. doi: 10.1186/s12986-020-00459-7.
- Giuliani A, Londin E, Ferracin M, Mensà E, Prattichizzo F, Ramini D, et al. Long-term exposure of human endothelial cells to metformin modulates miRNAs and isomiRs. Sci Rep. 2020;10(1):21782. doi: 10.1038/s41598-020-78871-5.
- Radhakrishnan R, Kowluru RA. Long noncoding RNA MALAT1 and regulation of the antioxidant defense system in diabetic retinopathy. Diabetes. 2021 Jan;70(1):227-239. doi: 10.2337/db20-0375.
- Wen Y, Chun Y, Lian ZQ, Yong ZW, Lan YM, Huan L, et al. circRNA‑0006896‑miR1264‑DNMT1 axis plays an important role in carotid plaque destabilization by regulating the behavior of endothelial cells in atherosclerosis. Mol Med Rep. 2021;23(5):311. doi: 10.3892/mmr.2021.1195.
- Xu X, Wu Z, Qiu H, Wu J. Circular RNA circPHC3 promotes cell death and apoptosis in human BMECs after oxygen glucose deprivation via miR-455-5p/TRAF3 axis in vitro. Neuropsychiatr Dis Treat. 2021;17:147-56. doi: 10.2147/NDT.S288669.
- Kleele T, Rey T, Winter J, Zaganelli S, Mahecic D, Perreten Lambert H, et al. Distinct fission signatures predict mitochondrial degradation or biogenesis. Nature. 2021;593(7859):435-439. doi: 10.1038/s41586-021-03510-6.
- Miyao M, Cicalese S, Kawai T, Cooper HA, Boyer MJ, Elliott KJ, et al. Involvement of senescence and mitochondrial fission in endothelial cell pro-inflammatory phenotype induced by angiotensin II. Int J Mol Sci. 2020;21(9):3112. doi: 10.3390/ijms21093112.
- Wang Q, Zhang M, Torres G, Wu S, Ouyang C, Xie Z, Zou MH. Metformin Suppresses Diabetes-Accelerated Atherosclerosis via the Inhibition of Drp1-Mediated Mitochondrial Fission. Diabetes. 2017 Jan;66(1):193-205. doi: 10.2337/db16-0915.
- Weikel KA, Cacicedo JM, Ruderman NB, Ido Y. Glucose and palmitate un couple AMPK from autophagy in human aortic endothelial cells. Am J Physiol Cell Physiol. 2015 Feb 1;308(3):C249-63. doi: 10.1152/ajpcell.00265.2014.
- Allende-Vega N, Marco Brualla J, Falvo P, Alexia C, Constantinides M, de Maudave AF, Coenon L, et al. Metformin sensiti–zes leukemic cells to cytotoxic lymphocytes by increasing expression of intercellular adhesion molecule-1 (ICAM-1). Sci Rep. 2022 Jan 25;12(1):1341. doi: 10.1038/s41598-022-05470-x. PMID: 35079096; PMCID: PMC8789909.
- Zhang M, Malik AB, Rehman J. Endothelial progenitor cells and vascular repair. Curr. Opin. Hematol. 2014, 21(3), 224-228. doi.org/10.1097/MOH.0000000000000041.
- Heinisch PP, Bello C, Emmert MY, Carrel T, Dreßen M, Hörer J, Winkler B, Luedi MM. Endothelial Progenitor Cells as Biomarkers of Cardiovascular Pathologies: A Narrative Review. Cells. 2022 May 18;11(10):1678. doi: 10.3390/cells11101678. PMID: 35626716; PMCID: PMC9139418.
- Yuan Q, Hu CP, Gong ZC, Bai YP, Liu SY, Li YJ, et al. Accelerated onset of senescence of endothelial progenitor cells in patients with type 2 diabetes mellitus: Role of dimethylarginine dimethylaminohydrolase 2 and asymmetric dimethylarginine. Biochem. Biophys. Res. Commun. 2015;458(4):869-876. doi.org/10.1016/j.bbrc.2015.02.050.
- Han X, Tao Y, Deng Y, Yu J, Sun Y, Jiang G. Metformin accelerates wound healing in type 2 diabetic db/db mice. Mol. Med. Rep. 2017; 16(6):8691-8698. doi.org/10.3892/mmr.2017.7707.
- Li WD, Li NP, Song DD, Rong JJ, Qian AM, Li XQ. Metformin inhibits endothelial progenitor cell migration by decreasing matrix metalloproteinases, MMP-2 and MMP-9, via the AMPK/mTOR/autophagy pathway. Int. J. Mol. Med. 2017;39(5):1262-1268. doi.org/10.3892/ijmm.2017.2929.
- Shang J, Zhang Y, Jiang Y, Li Z, Duan Y, Wang L, et al. NOD2 promotes endothelial-to-mesenchymal transition of glomerular endothelial cells via MEK/ERK signaling pathway in diabetic nephropathy. Biochem Biophys Res Commun. 2017;484(2):435-41. doi: 10.1016/j.bbrc.2017.01.155.
- Giordo R, Ahmed YMA, Allam H, Abusnana S, Pappalardo L, Nasrallah GK, et al. EndMT regulation by small RNAs in diabetes-associated fibrotic conditions: potential link with oxidative stress. Front Cell Dev Biol. 2021;9:683594. doi: 10.3389/fcell.2021.683594.
- Dallaglio K, Bruno A, Cantelmo AR, Esposito AI, Ruggiero L, Orecchioni S, et al. Paradoxic effects of metformin on endothelial cells and angiogenesis. Carcinogenesis. 35:1055-1066. doi: 10.1093/carcin/bgu001.
- Lee S. Update on SGLT2 inhibitors-new data released at the American Diabetes Association. Crit Pathw Cardiol. 2017 Sep;16(3):93-95. doi: 10.1097/HPC.0000000000000125.