Список литературы
1. Vila T., Romo J.A., Pierce C.G. et al. Targeting Candida albicans filamentation for antifungal drug development. Virulence. 2017;8(2):150-158. DOI: 10.1080/21505594.2016.1197444.
2. Alves A.M., Lopes B.O. et al. Characterization of Oral Candida spp. Biofilms in Children and Adults Carriers from Eastern Europe and South America. Antibiotics. 2023;12(5),797. https://doi.org/10.3390/antibiotics12050797.
3. Sivabalan S., Mahadevan S., Srinath M.V. Recurrent oral thrush. Indian J Pediatr. 2014;81(4):394-396. DOI: 10.1007/s12098-013-1201-x.
4. Mahajan B., Bagul N., Desai R. et al. Pseudomembranous Type of Oral Candidiasis is Associated with Decreased Salivary Flow Rate and Secretory Immunoglobulin A Levels. Mycopathologia. 2015;180(1-2):75-80. DOI: 10.1007/s11046-015-9874-5.
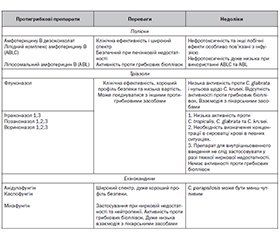
5. Guillermo Quindós, Sandra Gil-Alonso, Cristina Marcos-Arias et al. Therapeutic tools for oral candidiasis: Current and new antifungal drugs. Med Oral Patol Oral Cir Bucal. 2019;1;24(2):e172-80. doi: 10.4317/medoral.22978.
6. Hellstein J.W., Marek C.L. Candidiasis: Red and White Manifestations in the Oral Cavity. Head Neck Pathol. 2019;13(1):25-32. DOI: 10.1007/s12105-019-01004-6.
7. Li X.V., Leonardi I., Putzel G.G. et al. Immune regulation by fungal strain diversity in inflammatory bowel disease. Nature. 2022;603(7902):672-678. DOI: 10.1038/s41586-022-04502-w.
8. Lopes J.P., Lionakis M.S. Pathogenesis and virulence of Candida albicans. Virulence. 2022;13(1):89-121. DOI: 10.1080/21505594.2021.2019950.
9. Poissy J., Damonti L., Bignon A., Khanna N., Von Kietzell M. et al. Risk factors for candidemia: a prospective matched case-control study. Crit Care. 2020;24(1):109. DOI: 10.1186/s13054-020-2766-1.
10. Aitken J. Diversity, frequency and antifungal resistance of Candida species in patients with type 2 diabetes mellitus. Acta Оdontologica Scandinavica. 2018;76(8):1-7. DOI: 10.1080/00016357.2018.1484154.
11. Liyanage G., Gonapaladeniya M., Dissanayake T. Invasive Candidiasis Associated with Adenovirus Pneumonia. Case Rep Pediatr. 2021:2021:9905474. DOI: 10.1155/2021/9905474.
12. Henriquis M., Williams D. Pathogenesis and Virulence of Candida albicans аnd Candida glabrata. Pathogens. 2020;9(9):752; https://doi.org/10.3390/pathogens9090752.
13. Про затвердження Стандарту медичної допомоги «Раціональне застосування антибактеріальних і антифунгальних препаратів з лікувальною та профілактичною метою: Наказ МОЗ України від 23.08.2023 № 1513. https://moz.gov.ua.
14. Мазур І.П. Грибкові ураження слизової оболонки порожнини рота. Сучасна стоматологія. 2020. № 3. С. 72-77. DOI: 10.33295/1992-576X-2020-3-72.
15. Jovanovic M., Obradovic R. et al. The role of candida albicans on the development of stomatitis in patients wearing dentures. Sanamed. 2018;13(2):175-181. DOI: http://dx.doi.org/10.24125/sanamed.v13i2.236.
16. Ponde N.O. et al. Candida albicans biofilms and polymicrobial interactions. Сritical Reviews in Microbiology. 2021;47(1):91-111. DOI: 10.1080/1040841X.2020.1843400.
17. Richardson J.P., Ho J., Naglik J.R. Candida–Epithelial Interactions. J Fungi (Basel). 2018;4(1):22. DOI: 10.3390/jof4010022.
18. Verma А., Gaffen S.L., Swidergall M. Innate immunity Mucosal Candida infections. J. Fungi (Basel). 2017;3(4):60. DOI: 10.3390/jof3040060.
19. Borriello F., Zanoni F.I., Granucci F. Cellular and molecular mechanisms of antifungal innate immunity at epithelial barriers: The role of C-type lectin receptors. Eur. J. Immunol. 2020;50(3):317-325. DOI: 10.1002/eji.201848054.
20. Zhao Y., Perlin David S. Review of the Novel Echinocandin Antifungal Rezafungin: Animal Studies and Clinical Data. J Fungi (Basel). 2020;6(4):192. DOI: 10.3390/jof6040192.
21. Wu Y., Zeng Z., Guo Y. Candida albicans elicits protective allergic responses via platelet mediated T helper 2 and T helper 17 cell polarization. Immunity. 2021;54(11):2595-2610. DOI: 10.1016/j.immuni.2021.08.009.
22. Tzu-YuShao, David B. Haslam et al. Friendly fungi: symbiosis with commensal Candida albicans. Trends in Immunology. 202243(9): 706-717. https://doi.org/10.1016/j.it.2022.07.003.
23. Graus M.S. et al. Mannan Molecular Substructures Control Nanoscale Glucan Exposure in Candida. Cell Reports. 2018;24:2432-2442. https://doi.org/10.1016/j.celrep.2018.07.088.
24. Wang F., Yang Y., Li Z. et al. Mannan-Binding Lectin Regulates the Th17/Treg Axis Through JAK/STAT and TGF-β/SMAD Signaling Against Candida albicans Infection. J. of Inflammation Research. 2022;15:1797-1810. DOI: 10.2147/JIR.S344489.
25. Silao F., Ryman K., Jiang T., Ward M. et al. Glutamate dehydrogenase (Gdh2) — dependent alkalization is dispensable for escape from macrophages and virulence of Candida albicans. PLoS Pathog. 2020;16(9):e1008328. DOI: 10.1371/journal.ppat.1008328.
26. Tsui C. et al. Pathogenesis of Candida albicans biofilm. Pathogens and Disease. 2016;74(4). DOI: 10.1093/femspd/ftw018.
27. Adachi Т., Kawanishi N., Ichigaya N. et al. А Preliminary Pilot Study: Metabolomic Analysis of Saliva in Oral Candidiasis. Metabolites. 2022;12(12):1294.
28. Liotti F., Posteraro В. Development of a Multiplex PCR Platform for the Rapid Detection of Bacteria, Antibiotic Resistance, and Candida in Human Blood Samples. Front Cell Infect Microbiol. 2019;13:9:389. DOI: 10.3389/fcimb.2019.00389.
29. Schoenenberger-Arnaiz J.A., Aragones-Eroles A., Taberner-Bonastre P. et al. Therapeutic drug monitoring in fungal infections: The dawn of proactive monitoring. A narrative review. Biomedical Research and Clinical Practice. 2021;6:2-7. DOI: 10.15761/BRCP.1000223.
30. Fisher B.T., Boge C.L.K., Xiao R., Shuster S. et al. Multicenter Prospective Study of Biomarkers for Diagnosis of Invasive Candidiasis in Children and Adolescents. Clinical Infectious Diseases. 2022;75(2):248-259. doi: 10.1093/cid/ciab928.
31. Mauro C., Reynolds C.F., Maercker A., Skritskaya N. et al. Prolonged grief disorder: clinical utility of ICD-11 diagnostic guidelines. Psychol Med. 2019;49(5):861-867. DOI: 10.1017/S0033291718001563.
32. Williams D., Lewis M. Pathogenesis and treatment of oral candidosis. J Oral Microbiology. 2011:3:57-76. doi: 10.3402/jom.v3i0.5771.
33. Reinhardt L.C., Nascente P.S., Ribeiro J.S. et al. A single-center 18-year experience with oral candidiasis in Brazil: a retrospective study of 1,534 cases. Braz Oral Res. 2018:32:e92. doi: 10.1590/1807-3107bor-2018.vol32.0092.
34. Lewis M.A.O., Williams D.W. Diagnosis and management of oral candidosis. Br Dent J. 2017 Nov 10;223(9):675-681. doi: 10.1038/sj.bdj.2017.886.
35. Revie N.M., Iyer K.R., Robbins N., Cowen L.E. Antifungal Drug Resistance: evolution, mechanisms and impact. Curr Opin Microbiol. 2018;45:70-76. DOI: 10.1016/j.mib.2018.02.005.
36. Пухлик С.М., Тагунова І.К., Андрєєв О.В. Роль грибкової інфекції при хронічному запаленні піднебіння мигдаликів та можливості лікування. Оториноларингология. Восточная Европа. 2017. (1). С. 123-125.
37. Mueller S.W., Kedzior S.K., Miller M.A. et al. An overview of current and emerging antifungal pharmacotherapy for invasive fungal infections. Expert Opin Pharmacother. 2021;22(10):1355-1371. DOI: 10.1080/14656566.2021.1892075.
38. Pappas P.G., Kauffman C.A., Andes D.R. et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clinical Infectious Diseases. 2016;62(4): e1-e50. https://doi.org/10.1093/cid/civ933.
39. Hope W.W, Castagnola E., Groll A.H, Roilides E., Akova M., Arendrup M.C. et. al. ESCMID guideline for the diagnosis and management of Candida diseases 2012: prevention and management of invasive infections in neonates and children caused by Candida spp. Clin Microbiol Infect. 2012;Suppl 7:38-52. DOI: 10.1111/1469-0691.12040.
40. Lyu X., Zhao C., Yan Z.M., Hua H. Efficacy of nystatin for the treatment of oral candidiasis: a systematic review and meta-analysis. Drug Des Devel Ther. 2016 Mar 16;10:1161-71. DOI: 10.2147/DDDT.S100795.
41. Garcia-Cuesta C., Sarrion-Pérez M.G., Bagán J.V. Current treatment of oral candidiasis: A literature review. J Clin Exp Dent. 2014;6(5):e576-82. http://dx.doi.org/10.4317/jced.51798.
42. Kaplan Y.C., Koren G., Ito S., Bozzo P. Fluconazole use during breastfeeding. Can Fam Physician. 2015 Oct;61(10):875-6.
43. Kuunda S., Adeoti K., Munir M., Giusti Al., Refinetti P., Otu A. et al. Application of probiotic-based multicomponents for human, animal and ecosystem health: concepts, methodologies and mechanisms of action. Microorganisms. 2022;10 (9):1700. https://doi.org/10.3390/microorganisms10091700.
44. Jorgensen M.R., Kragelund C., Jensen P.O. et al. Probiotic Lactobacillus reuteri has antifungal effects on oral Candida species in vitro. J Oral Microbiol. 2017;9(1):1274582. doi: 10.1080/20002297.2016.1274582.
45. Denkova R., Yanakieva V., Denkova Z., Nikolova V., Radeva V. In vitro inhibitory activity of Bifidobacterium and Lactobacillus strains against Candida albicans. Bulgarian Journal of Veterinary Medicine. 2013;16 (3):186-197. https://cabidigitallibrary.org/terms.
46. Chew S.Y., Cheah Y.K., Seow H.F., Sandai D., Than L.T. In vitro modulation of probiotic bacteria on the biofilm of Candida glabrata. Anaerobe. 2015;34:132-138. DOI: 10.1016/j.anaerobe.2015.05.009.
47. Guarner F., Sanders M.E., Szajewska H. et al. Probiotics and prebiotics WGO Global Guideline. World Gastroenterology Organisation, 2023. 52 р.
48. Swanson K.S., Gibson G.R., Hutkins R., Reimer R.A. et al. The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of synbiotics. Nat Rev Gastroenterol Hepatol. 2020;17(11):687-701. DOI: 10.1038/s41575-020-0344-2.
49. Yadav M.K., Kumari I., Singh B. et al. Probiotics, prebiotics and synbiotics: Safe options for next-generation therapeutics. Appl Microbiol. Biotechnol. 2022;106(2):505-521. doi: 10.1007/s00253-021-11646-8.
50. Centurion F., Basit A.W, Liu J., Gaisford S. et al. Nanoencapsulation for Probiotic Delivery. ACS Nano. 2021;15(12):18653-18660. DOI: 10.1021/acsnano.1c09951.
51. Su Y., Zheng X., Zhao Q. et al. Spray drying of Lactobacillus rhamnosus GG with calcium-containing protectant for enhanced viabi–lity. Powder Technology. 2019;358:87-94. https://doi.org/10.1016/j.powtec.2018.09.082.
52. Rajam R., Subramanian P. Encapsulation of probiotics: past, present and future. J Basic Appl Sci. 2022;11:46. https://doi:org/10.1186/s43088-022-00228-w.
53. Mundula T., Ricci F., Barbetta B. et al. Effect of Probiotics on Oral Candidiasis: A Systematic Review and Meta-Analysis Nutrients. 2019;11(10):2449. https://doi.org/10.3390/nu11102449.
54. Li D., Li Q., Liu Ch., Lin M., Li X. et al. Efficacy and safety of probiotics in the treatment of Candida-associated stomatitis. Mycoses. 2014;57(3):141-6. DOI: 10.1111/myc.12116.
55. Doppalapudi R., Vundavalli S., Prabhat M.P. Effect of probio–tic bacteria on oral Candida in head- and neckradiotherapy patients: A randomized clinical trial. Journal of Cancer Research and Therapeutics. 2020; 16(3):470-477. DOI: 10.4103/jcrt.JCRT.334.18.
56. Фесенко В.І., Фесенко В.І. Загальнооздоровча терапія при грибковому ураженні слизової оболонки порожнини рота. Středoevropský věstník pro vědu a výzkum. 2021;4:15-20. http://czvestnic.info/ojs/index.php/cz_ojs/article/view/81.