Журнал «Здоровье ребенка» Том 19, №7, 2024
Вернуться к номеру
Автозапальні захворювання. Частина 1: концепт, класифікація, імунобіологія, діагностика
Авторы: Шварацька О.В., Калічевська М.В., Клименко О.В., Таран О.М., Клімова О.В., Віленський Я.В., Плеханова Т.М., Мавропуло Т.К.
Дніпровський державний медичний університет, м. Дніпро, Україна
Рубрики: Педиатрия/Неонатология
Разделы: Справочник специалиста
Версия для печати
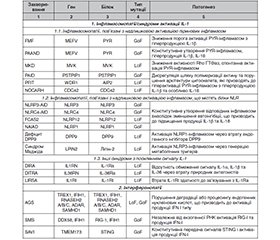
Системні автозапальні захворювання (САЗЗ) — це група спадкових моногенних захворювань, що характеризуються порушеннями регуляції вродженого імунітету, які спричиняють надмірну активацію шляхів запалення. Водночас наразі визнається, що молекулярні механізми, характерні для автозапалення, також залучені до патогенезу низки автоімунних та імунодефіцитних станів. Метою цього наукового огляду була систематизація актуальних уявлень про автозапальні захворювання для підвищення обізнаності лікарів практичної медицини щодо них, яка є суттєво меншою, ніж щодо інших категорій імунної дисфункції. Пошук інформації за останні 10 років здійснювався у базах даних Web of Science, Scopus, PubMed Central®, Google Scholar за такими ключовими словами: autoinflammatory diseases, autoinflammatory syndromes, autoinflammation. В огляді висвітлено історичну еволюцію уявлень про імунопатогенез автозапалення від часу впровадження концепту 1999 року: від інтерлейкін(IL)-1-центричної парадигми до визначення значущої ролі інших сигнальних шляхів; розглянуто місце автозапалення у спектрі імунологічних розладів. Також наведено актуальні наукові дані про імунобіологічну основу автозапалення — інфламасомний, інтерфероновий та залежний від ядерного фактора каппа В (NFκB) сигнальні шляхи, з висвітленням ролі внутрішньоклітинних сенсорних білків, інфламасом, газдерміну D, IL-1β, IL-18 та IL-36, NFκB, фактора некрозу пухлини, інтерферонів 1-го типу тощо. Відповідно до основного молекулярного патогенезу захворювання нещодавно було запропоновано виокремлювати наступні класифікаційні категорії САЗЗ: інфламасомопатії й інші синдроми посилення сигналу IL-1, інтерферонопатії, релопатії, розлади фолдингу білка та синдроми стресу ендоплазматичного ретикулуму, інші розлади цитокінової сигналізації та комплементопатії. В огляді також обговорено діагностичні виклики та подано сучасні наукові рекомендації щодо діагностики САЗЗ з висвітленням відмінних рис класичних автозапальних розладів і наявного потенціалу діагностичних тестів.
Systemic autoinflammatory diseases (SAIDs) are a group of inherited monogenic diseases characterized by dysregulated innate immunity leading to excessive activation of inflammatory pathways. Recently, some molecular mechanisms typical for autoinflammation have also been recognized in the pathogenesis of several autoimmune and immunodeficiency states. This scientific review aimed to systematize current ideas about autoinflammatory diseases to increase medical professionals’ awareness regarding the issue, which is significantly lower than that of other categories of immune dysfunction. We performed a focused search over the Web of Science, Scopus, PubMed Central®, Google Scholar databases over the past 10 years using the keywords “autoinflammatory diseases”, “autoinflammatory syndromes”, “autoinflammation”. The review reflects the historical evolution of scientific views on the immunopathogenesis of autoinflammation since the introduction of the concept in 1999: from the interleukin (IL)-1-centered paradigm to recognition of the significant role of other signaling pathways. Further, we discuss the place of autoinflammation in the spectrum of immunological disorders and present current scientific data on the immunobiological basis of autoinflammation. In particular, we review how the innate immune system triggers inflammation within the inflammasome, interferon and nuclear factor kappa B (NF-κB) signaling pathways, highlighting the role of intracellular sensor proteins, inflammasomes, gasdermin D, IL-1β, IL-18 and IL-36, NF-κB, tumor necrosis factor, type 1 interferons, and others. Based on the underlying molecular pathogenesis, the following classification categories of SAIDs have been suggested recently: inflammasomopathies and other enhanced IL-1 signaling syndromes, interferonopathies, relopathies, protein misfolding diseases/endoplasmic reticulum stress syndromes, other cytokine-signaling disorders and complementopathies. The review also discusses diagnostic challenges and presents current scientific recommendations for the diagnosis of SAIDs, highlighting the distinguishing features of the classic autoinflammatory disorders and the existing potential of diagnostic tests.
автозапалення; автозапальні захворювання; інфламасомопатії; інтерферонопатії; релопатії; огляд
autoinflammation; autoinflammatory diseases; inflammasomopathies; interferonopathies; relopathies; review
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- de Jesus AA, Goldbach-Mansky R. Genetically defined autoinflammatory diseases. Oral Dis. 2016 Oct;22(7):591-604. doi: 10.1111/odi.12448.
- Li Y, Yu M, Lu M. Pathophysiology, clinical manifestations and current management of IL-1 mediated monogenic systemic autoinflammatory diseases, a literature review. Pediatr Rheumatol Online J. 2022 Oct 17;20(1):90. doi: 10.1186/s12969-022-00728-0.
- Sarrabay G, Barat-Houari M, Annakib S, Touitou I. The autoinflammatory diseases: a fashion with blurred boundaries! Semin Immunopathol. 2015 Jul;37(4):359-62. doi: 10.1007/s00281-015-0495-3.
- Kul Cinar O, Putland A, Wynne K, Eleftheriou D, Brogan PA. Hereditary Systemic Autoinflammatory Diseases: Therapeutic Stratification. Front Pediatr. 2022 Apr 28;10:867679. doi: 10.3389/fped.2022.867679.
- Zhang J, Lee PY, Aksentijevich I, Zhou Q. How to Build a Fire: The Genetics of Autoinflammatory Diseases. Annu Rev Genet. 2023 Nov 27;57:245-274. doi: 10.1146/annurev-genet-030123-084224.
- Krainer J, Siebenhandl S, Weinhäusel A. Systemic autoinflammatory diseases. J Autoimmun. 2020 May;109:102421. doi: 10.1016/j.jaut.2020.102421.
- Moghaddas F. Monogenic autoinflammatory disorders: beyond the periodic fever. Intern Med J. 2020 Feb;50(2):151-164. doi: 10.1111/imj.14414.
- Bousfiha A, Jeddane L, Picard C, et al. The 2017 IUIS phenotypic classification for primary immunodeficiencies. J Clin Immunol. 2018 Jan;38(1):129-143. doi: 10.1007/s10875-017-0465-8.
- Toplak N, Frenkel J, Ozen S, Lachmann HJ, et al. An international registry on autoinflammatory diseases: the Eurofever experience. Ann Rheum Dis. 2012 Jul;71(7):1177-82. doi: 10.1136/annrheumdis-2011-200549.
- Ancient missense mutations in a new member of the RoRet gene family are likely to cause familial Mediterranean fever. The International FMF Consortium. Cell. 1997 Aug 22;90(4):797-807. doi: 10.1016/s0092-8674(00)80539-5.
- McDermott MF, Aksentijevich I, Galon J, et al. Germline mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, define a family of dominantly inherited autoinflammatory syndromes. Cell. 1999;97(1):133-144. doi: 10.1016/S0092-8674(00)80721-7.
- Canna SW, Goldbach-Mansky R. New monogenic autoinflammatory diseases — a clinical overview. Semin Immunopathol. 2015 Jul;37(4):387-94. doi: 10.1007/s00281-015-0493-5.
- Nigrovic PA, Lee PY, Hoffman HM. Monogenic autoinflammatory disorders: Conceptual overview, phenotype, and clinical approach. J Allergy Clin Immunol. 2020 Nov;146(5):925-937. doi: 10.1016/j.jaci.2020.08.017.
- Kastner DL, Aksentijevich I, Goldbach-Mansky R. Autoinflammatory disease reloaded: a clinical perspective. Cell. 2010 Mar 19;140(6):784-90. doi: 10.1016/j.cell.2010.03.002.
- Masters SL, Simon A, Aksentijevich I, Kastner DL. Horror autoinflammaticus: the molecular pathophysiology of autoinflammatory di–sease. Annu Rev Immunol. 2009;27:621-68. doi: 10.1146/annurev.immunol.25.022106.141627.
- Hoffman HM, Mueller JL, Broide DH, Wanderer AA, Kolodner RD. Mutation of a new gene encoding a putative pyrin-like protein causes familial cold autoinflammatory syndrome and Muckle-Wells syndrome. Nat Genet. 2001 Nov;29(3):301-5. doi: 10.1038/ng756.
- Hoffman HM, Wanderer AA, Broide DH. Familial cold autoinflammatory syndrome: phenotype and genotype of an autosomal dominant periodic fever. J Allergy Clin Immunol. 2001 Oct;108(4):615-20. doi: 10.1067/mai.2001.118790.
- Hoffman HM, Broderick L. The role of the inflammasome in patients with autoinflammatory diseases. J Allergy Clin Immunol. 2016 Jul;138(1):3-14. doi: 10.1016/j.jaci.2016.05.001.
- Lin B, Goldbach-Mansky R. Pathogenic insights from genetic causes of autoinflammatory inflammasomopathies and interferonopathies. J Allergy Clin Immunol. 2022 Mar;149(3):819-832. doi: 10.1016/j.jaci.2021.10.027.
- Lamkanfi M, Dixit VM. In Retrospect: The inflammasome turns 15. Nature. 2017 Aug 30;548(7669):534-535. doi: 10.1038/548534a.
- Martinon F, Burns K, Tschopp J. The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Mol Cell. 2002 Aug;10(2):417-26. doi: 10.1016/s1097-2765(02)00599-3.
- Broderick L, De Nardo D, Franklin BS, Hoffman HM, Latz E. The inflammasomes and autoinflammatory syndromes. Annu Rev Pathol. 2015;10:395-424. doi: 10.1146/annurev-pathol-012414-040431.
- Jesus AA, Goldbach-Mansky R. IL-1 blockade in autoinflammatory syndromes. Annu Rev Med. 2014;65:223-44. doi: 10.1146/annurev-med-061512-150641.
- Alehashemi S, Goldbach-Mansky R. Human Autoinflammatory Diseases Mediated by NLRP3-, Pyrin-, NLRP1-, and NLRC4-Inflammasome Dysregulation Updates on Diagnosis, Treatment, and the Respective Roles of IL-1 and IL-18. Front Immunol. 2020 Aug 25;11:1840. doi: 10.3389/fimmu.2020.01840.
- Schnappauf O, Chae JJ, Kastner DL, Aksentijevich I. The Pyrin Inflammasome in Health and Disease. Front Immunol. 2019 Aug 7;10:1745. doi: 10.3389/fimmu.2019.01745.
- Kawakami A, Endo Y, Koga T, Yoshiura KI, Migita K. Autoinflammatory disease: clinical perspectives and therapeutic strategies. Inflamm Regen. 2022 Dec 2;42(1):37. doi: 10.1186/s41232-022-00217-7.
- Almeida de Jesus A, Goldbach-Mansky R. Monoge–nic autoinflammatory diseases: concept and clinical manifestations. Clin Immunol. 2013 Jun;147(3):155-74. doi: 10.1016/j.clim.2013.03.016.
- Goldbach-Mansky R. Immunology in clinic review series; focus on autoinflammatory diseases: update on monogenic autoinflammatory diseases: the role of interleukin (IL)-1 and an emerging role for cytokines beyond IL-1. Clin Exp Immunol. 2012 Mar;167(3):391-404. doi: 10.1111/j.1365-2249.2011.04533.x.
- Pathak S, McDermott MF, Savic S. Autoinflammatory diseases: update on classification diagnosis and management. J Clin Pathol. 2017 Jan;70(1):1-8. doi: 10.1136/jclinpath-2016-203810.
- Rood JE, Behrens EM. Inherited Autoinflammatory Syndromes. Annu Rev Pathol. 2022 Jan 24;17:227-249. doi: 10.1146/annurev-pathmechdis-030121-041528.
- Doria A, Zen M, Bettio S, Gatto M, et al. Autoinflammation and autoimmunity: bridging the divide. Autoimmun Rev. 2012 Nov;12(1):22-30. doi: 10.1016/j.autrev.2012.07.018.
- Navegantes KC, de Souza Gomes R, Pereira PAT, et al. Immune modulation of some autoimmune diseases: the critical role of macrophages and neutrophils in the innate and adaptive immunity. J Transl Med. 2017 Feb 15;15(1):36. doi: 10.1186/s12967-017-1141-8.
- Wang L, Wang FS, Gershwin ME. Human autoimmune diseases: a comprehensive update. J Intern Med. 2015 Oct;278(4):369-95. doi: 10.1111/joim.12395.
- Havnaer A, Han G. Autoinflammatory Disorders: A Review and Update on Pathogenesis and Treatment. Am J Clin Dermatol. 2019 Aug;20(4):539-564. doi: 10.1007/s40257-019-00440-y.
- Zhou Q, Aksentijevich I, Wood GM, et al. Brief Report: Cryopyrin-Associated Periodic Syndrome Caused by a Myeloid-Restricted Somatic NLRP3 Mutation. Arthritis Rheumatol. 2015 Sep;67(9):2482-6. doi: 10.1002/art.39190.
- Rowczenio DM, Trojer H, Omoyinmi E, et al. Brief Report: Association of Tumor Necrosis Factor Receptor-Associated Periodic Syndrome With Gonosomal Mosaicism of a Novel 24-Nucleotide TNFRSF1A Deletion. Arthritis Rheumatol. 2016 Aug;68(8):2044-9. doi: 10.1002/art.39683.
- de Inocencio J, Mensa-Vilaro A, Tejada-Palacios P, et al. Somatic NOD2 mosaicism in Blau syndrome. J Allergy Clin Immunol. 2015 Aug;136(2):484-7.e2. doi: 10.1016/j.jaci.2014.12.1941.
- Shinar Y, Tohami T, Livneh A, et al. Acquired familial Mediterranean fever associated with a somatic MEFV mutation in a patient with JAK2 associated post-polycythemia myelofibrosis. Orphanet J Rare Dis. 2015 Jun 30;10:86. doi: 10.1186/s13023-015-0298-6.
- Amarante-Mendes GP, Adjemian S, Branco LM, et al. Pattern Recognition Receptors and the Host Cell Death Molecular Machinery. Front Immunol. 2018 Oct 16;9:2379. doi: 10.3389/fimmu.2018.02379.
- Davis BK, Wen H, Ting JP. The inflammasome NLRs in immunity, inflammation, and associated diseases. Annu Rev Immunol. 2011;29:707-35. doi: 10.1146/annurev-immunol-031210-101405.
- Zheng D, Liwinski T, Elinav E. Inflammasome activation and regulation: toward a better understanding of complex mechanisms. Cell Discov. 2020 Jun 9;6:36. doi: 10.1038/s41421-020-0167-x.
- Hikima J, Morimoto N. Evolutive aspects of inflammasomes. In: Pelegrin P, editor. Inflammasome Biology. Academic Press; 2023. P. 235-245. doi: 10.1016/B978-0-323-91802-2.00013-X.
- Motta V, Soares F, Sun T, Philpott DJ. NOD-like receptors: versatile cytosolic sentinels. Physiol Rev. 2015 Jan;95(1):149-78. doi: 10.1152/physrev.00009.2014.
- Lu A, Magupalli VG, Ruan J, et al. Unified polymerization mecha–nism for the assembly of ASC-dependent inflammasomes. Cell. 2014 Mar 13;156(6):1193-1206. doi: 10.1016/j.cell.2014.02.008.
- Shi J, Zhao Y, Wang K, et al. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature. 2015 Oct 29;526(7575):660-5. doi: 10.1038/nature15514.
- Awad F, Assrawi E, Louvrier C, et al. Inflammasome biology, molecular pathology and therapeutic implications. Pharmacol Ther. 2018 Jul;187:133-149. doi: 10.1016/j.pharmthera.2018.02.011.
- La Bella S, Di Ludovico A, Di Donato G, et al. The pyrin inflammasome, a leading actor in pediatric autoinflammatory diseases. Front Immunol. 2024 Jan 5;14:1341680. doi: 10.3389/fimmu.2023.1341680.
- Akdis M, Aab A, Altunbulakli C, Azkur K, et al. Interleukins (from IL-1 to IL-38), interferons, transforming growth factor β, and TNF-α: Receptors, functions, and roles in diseases. J Allergy Clin Immunol. 2016 Oct;138(4):984-1010. doi: 10.1016/j.jaci.2016.06.033.
- Jarosz-Griffiths HH, Holbrook J, Lara-Reyna S, McDermott MF. TNF receptor signalling in autoinflammatory diseases. Int Immunol. 2019 Sep 18;31(10):639-648. doi: 10.1093/intimm/dxz024.
- Belkaya S, Michailidis E, Korol CB, et al. Inherited IL-18BP deficiency in human fulminant viral hepatitis. J Exp Med. 2019 Aug 5;216(8):1777-1790. doi: 10.1084/jem.20190669.
- Zhou L, Todorovic V. Interleukin-36: Structure, Signaling and Function. Adv Exp Med Biol. 2021;21:191-210. doi: 10.1007/5584_2020_488.
- Boucher D, Monteleone M, Coll RC, et al. Caspase-1 self-clea–vage is an intrinsic mechanism to terminate inflammasome activity. J Exp Med. 2018 Mar 5;215(3):827-840. doi: 10.1084/jem.20172222.
- Zhang K, Huang Q, Li X, et al. The cGAS-STING pathway in viral infections: a promising link between inflammation, oxidative stress and autophagy. Front Immunol. 2024 Feb 15;15:1352479. doi: 10.3389/fimmu.2024.1352479.
- Fan YM, Zhang YL, Luo H, Mohamud Y. Crosstalk between RNA viruses and DNA sensors: Role of the cGAS-STING signalling pathway. Rev Med Virol. 2022 Sep;32(5):e2343. doi: 10.1002/rmv.2343.
- Xie F, Zhu Q. The regulation of cGAS-STING signaling by RNA virus-derived components. Virol J. 2024 May 1;21(1):101. doi: 10.1186/s12985-024-02359-1.
- An J, Marwaha A, Laxer RM. Autoinflammatory Diseases: A Review. J Rheumatol. 2024 Sep 1;51(9):848-861. doi: 10.3899/jrheum.2023-1209.
- Maalouly M, Saade S, Kurban M. Autoinflammatory diseases: what is behind them and what is new? Dermatol Reports. 2022 Dec 29;15(2):9625. doi: 10.4081/dr.2023.9625.
- Cowen EW, Goldbach-Mansky R. DIRA, DITRA, and new insights into pathways of skin inflammation: what’s in a name? Arch Dermatol. 2012 Mar;148(3):381-4. doi: 10.1001/archdermatol.2011.3014.
- Kutukculer N, Topyildiz E, Berdeli A, et al. Four diseases, PLAID, APLAID, FCAS3 and CVID and one gene (PHOSPHOLIPASE C, –GAMMA-2; PLCG2): Striking clinical phenotypic overlap and diffe–rence. Clin Case Rep. 2021 Mar 2;9(4):2023-2031. doi: 10.1002/ccr3.3934.
- Neves JF, Doffinger R, Barcena-Morales G, et al. Novel PLCG2 Mutation in a Patient With APLAID and Cutis Laxa. Front Immunol. 2018 Dec 14;9:2863. doi: 10.3389/fimmu.2018.02863.
- Bordon Y. The autoinflammatory disease APLAID is driven by G-CSF. Nat Rev Immunol. 2023 May;23(5):271. doi: 10.1038/s41577-023-00880-y.
- Federici S, Gattorno M. A practical approach to the diagnosis of autoinflammatory diseases in childhood. Best Pract Res Clin Rheumatol. 2014 Apr;28(2):263-76. doi: 10.1016/j.berh.2014.05.005.
- Gattorno M, Sormani MP, D’Osualdo A, et al. A diagnostic score for molecular analysis of hereditary autoinflammatory syndromes with periodic fever in children. Arthritis Rheum. 2008 Jun;58(6):1823-32. doi: 10.1002/art.23474.
- Gattorno M, Hofer M, Federici S, et al. Classification criteria for autoinflammatory recurrent fevers. Ann Rheum Dis. 2019 Aug;78(8):1025-1032. doi: 10.1136/annrheumdis-2019-215048.
- Federici S, Sormani MP, Ozen S, et al. Evidence-based provisional clinical classification criteria for autoinflammatory periodic fevers. Ann Rheum Dis. 2015 May;74(5):799-805. doi: 10.1136/annrheumdis-2014-206580.
- Romano M, Arici ZS, Piskin D, et al. The 2021 EULAR/American College of Rheumatology Points to Consider for Diagnosis, Management and Monitoring of the Interleukin-1 Mediated Autoinflammatory Diseases: Cryopyrin-Associated Periodic Syndromes, Tumour Necrosis Factor Receptor-Associated Periodic Syndrome, Mevalonate Kinase Deficiency, and Deficiency of the Interleukin-1 Receptor Antagonist. Arthritis Rheumatol. 2022 Jul;74(7):1102-1121. doi: 10.1002/art.42139.
- Ozen S. Update in familial Mediterranean fever. Curr Opin Rheumatol. 2021 Sep 1;33(5):398-402. doi: 10.1097/BOR.0000000000000821.
- Cetin Gedik K, Lamot L, Romano M, et al. The 2021 European Alliance of Associations for Rheumatology/American College of Rheumato–logy points to consider for diagnosis and management of autoinflammatory type I interferonopathies: CANDLE/PRAAS, SAVI and AGS. Ann Rheum Dis. 2022 May;81(5):601-613. doi: 10.1136/annrheumdis-2021-221814.
- Papa R, Rusmini M, Volpi S, et al. Next generation sequencing panel in undifferentiated autoinflammatory diseases identifies patients with colchicine-responder recurrent fevers. Rheumatology (Oxford). 2020 Feb 1;59(2):344-360. doi: 10.1093/rheumatology/kez270.
- Batlle-Masó L, Mensa-Vilaró A, Solís-Moruno M, et al. Genetic diagnosis of autoinflammatory disease patients using clinical exome sequencing. Eur J Med Genet. 2020 May;63(5):103920. doi: 10.1016/j.ejmg.2020.103920.
- Kant B, Carbo EC, Kokmeijer I, et al. Gene Mosaicism Screening Using Single-Molecule Molecular Inversion Probes in Routine Diagnostics for Systemic Autoinflammatory Diseases. J Mol Diagn. 2019 Nov;21(6):943-950. doi: 10.1016/j.jmoldx.2019.06.009.
- Harrison SR, McGonagle D, Nizam S, et al. Anakinra as a diagnostic challenge and treatment option for systemic autoinflammatory disorders of undefined etiology. JCI Insight. 2016 May 5;1(6):e86336. doi: 10.1172/jci.insight.86336.