Журнал «Медицина неотложных состояний» Том 21, №1, 2025
Вернуться к номеру
Еволюція клінічних та генетичних концепцій кардіоміопатій
Авторы: Ковальова О.М. (1), Ніконов В.В. (1), Іванченко С.В. (1), Літвинова А.М. (1), В’юн Т.І. (1), Федота О.М. (2)
(1) - Харківській національний медичний університет, м. Харків, Україна
(2) - ТОВ «AMS», м. Харків, Україна
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
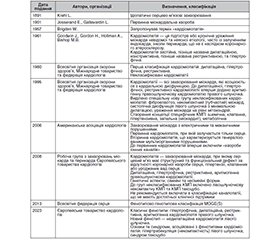
Наведено визначення та класифікації кардіоміопатій в історичному аспекті на підставі аналізу бази даних на платформах PubMed, Web of Science, Scopus та Google Scholar з використанням відповідних ключових термінів. Відзначено, що впровадження високотехнологічних методів досліджень супроводжується створенням концепцій кардіоміопатій з встановленням етіологічних та патогенетичних ланок, що трансформуються в клінічні ознаки, які потребують стратифікації, оцінки факторів ризику, прогнозу. Проаналізовано діагностичну цінність структурно-функціональних аномалій серця для ранжування класичних фенотипів дилатаційної, гіпертрофічної, рестриктивної кардіоміопатій та аритмогенної кардіомопатії правого шлуночка. Подано опис нового фенотипу недилатаційної кардіоміопатії лівого шлуночка та синдромів, асоційованих з фенотипами кардіоміопатій: гіпертрабекуляції (некомпактність) лівого шлуночка, синдрому такоцубо. Наведено аналіз можливостей генетичних досліджень щодо встановлення первинних етіологічних факторів ураження міокарда, формування груп ризику. Зазначено, що передумовами застосування методів лабораторної генетики у практичні роботі є проведення генетичного аналізу на рівні родини та особи, із встановленням генеалогічних, статево-вікових, фенотипових й інших особливостей хворих та їхніх родичів. Визначено, що інтерпретація результатів комплексного клінічного обстеження та повного генетичного аналізу надає фундаментальну базу та практичні інструменти для стратифікації симптомів і диференціації кардіоміопатій, своєчасного впровадження заходів для усунення аритмій, запобігання раптовій серцевій смерті у хворих, надання консультацій стосовно прогностичних та превентивних медичних рекомендацій членам родини.
The definitions and classifications of cardiomyopathies are presented from a historical perspective based on an analysis of databases on platforms such as PubMed, Web of Science, Scopus, and Google Scholar, using appropriate keywords. It is noted that the implementation of high-tech research methods is accompanied by the creation of concepts of cardiomyopathies, establishing etiological and pathogenetic links that are being transformed into clinical signs, which require stratification, risk factor assessment, and prognosis. The diagnostic value of structural and functional heart anomalies for ranking classical phenotypes of dilated, hypertrophic, restrictive cardiomyopathies, and arrhythmogenic right ventricular cardiomyopathy is аnalyzed. A description is provided of a new phenotype of non-dilated left ventricular cardiomyopathy and syndromes associated with cardiomyopathy phenotypes such as left ventricular hypertrabeculation (non-compaction) and takotsubo syndrome. The possibilities of genetic research in determining the primary etiological factors of myocardial damage, risk groups for-ming are analyzed. It is noted that the prerequisite for the application of laboratory genetic methods in practical work is genetic analysis at the family and individual level with establishing genealogical, sex-age, phenotypic, and other characteristics of patients and their relatives. It is determined that the interpretation of the results of a comprehensive clinical examination and complete genetic testing provides a fundamental base and practical tools for the stratification of symptoms and differentiation of cardiomyopathies, timely implementation of measures to eliminate arrhythmias, prevent sudden cardiac death in patients, and for providing consultation on prognostic and preventive medical recommendations to family members.
кардіоміопатії; класифікації; генетичний аналіз; сімейний анамнез; історія; огляд
cardiomyopathies; classifications; genetic analysis; fa-mily anamnesis; history; review
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Braunwald E. Cardiomyopathies. An Overview. Circ Res. 2017 Sep 15;121(7):711-721. doi: 10.1161/CIRCRESAHA.117.311812.
- Brigden W. Uncommon myocardial diseases: the non-coronary cardiomyopathies. Lancet. 1957 Dec 14;273(7007):1179-84. doi: 10.1016/s0140-6736(57)90159-9.
- Goodwin JF, Gordon H, Hollman A, Bishop MB. Clinical aspects of cardiomyopathy. Br Med J. 1961 Jan 14;1(5219):69-79. doi: 10.1136/bmj.1.5219.69.
- Brandenburg RO, Chazov E, Cherian G, False AO, Grosgogeat Y, Kawai C, et al. Report of the WHO/ISFC task force on the definition and classification of cardiomyopathies. Br Heart J. 1980 Dec;44(6):672-3. doi: 10.1136/hrt.44.6.672.
- Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O’Connell J, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology task force on the definition and classification of cardiomyopathies. Circulation. 1996 Mar 1;93(5):841-2. doi: 10.1161/01.cir.93.5.841.
- Marcus F, Fontaine G, Guiraudon G, Frank R, Laurenceau J, Malergue C, et al. Right ventricular dysplasia: a report of 24 adult ca-ses. Circulation. 1982 Feb;65(2):384-98. doi: 10.1161/01.cir.65.2.384.
- Basso C, Thiene G, Corrado D, Angelini A, Nava A, Valente M. Arrhythmogenic right ventricular cardiomyopathy. Dysplasia, dystrophy, or myocarditis? Circulation. 1996;94:983-991. doi: 10.1161/01.CIR.94.5.983.
- McKenna WJ, Thiene G, Nava A, Fontaliron F, Blomstrom-Lundquist G, Fontaine G, еt al. Diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Task Force of the Working Group Myocardial and Pericardial Disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology. Br Heart J. 1994 Mar;71(3):215-8. doi: 10.1136/hrt.71.3.215.
- Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J. 2010;31:806-14. https://doi.org/10.1093/ eurheartj/ehq025.
- Perry M, Elliott AA, Asimaki A, Basso C, Bauce B, Brooke MA, et al. Definition and treatment of arrhythmogenic cardiomyopathy: An updated expert panel report. Eur J Heart Fail. 2019 Aug;21(8):955-964. doi: 10.1002/ejhf.1534.
- Maron B, Towbin J, Thiene G, Antzelevitch C, Corrado D, Arnett D, et al. Contemporary definitions and classification of the cardiomyopathies. An American Heart Association scientific statement from the council on clinical cardiology, heart failure and transplantation committee;quality of care and outcomes research and functional genomics and translational biology interdisciplinary working groups;and council on epidemiology and prevention. Circulation. 2006 Apr 11;113(14):1807-16. doi: 10.1161/CIRCULATIONAHA.106.174287.
- Ackerman MJ, Priori SG, Willems S, Berul C, Brugada R, Calkins H, et al. HRS/EHRA Expert Consensus Statement on the State of Genetic Testing for Channelopathies and Cardiomyopathies. Europace. 2011 Aug;13(8):1077-109. doi: 10.1093/europace/eur245.
- Elliott P, Anderson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, et al. Classification of cardiomyopathies: a position statement from the European working group on myocardial and pericardial diseases. Eur Heart J. 2008 Jan;29(2):270-6. doi: 10.1093/eurheartj/ehm342.
- Gersh B, Maron B, Bonow R, Dearani J, Fifer M, Link S, et al. 2011 ACCF/AHA Guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American college of cardiology foundation/American heart association task force of practice guidelines. J Am Coll Cardiol. 2011 Dec 13;58(25):2703-38. doi: 10.1016/j.jacc.2011.10.825.
- Authors/Task Force members; Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35:2733-2779. https://doi.org/10.1093/eurheartj/ehu284.
- Ciarambino T, Menna G, Sansone G, Giordano M. Cardiomyopathies. An Overview Int J Mol Sci. 2021 Jul 19;22(14):7722. doi: 10.3390/ijms22147722.
- Llamas-Esperón GA, Llamas-Delgado G. Hypertrophic cardiomyopathy. Proposal for a new classification. Arch Cardiol Mex. 2022;92(3):377-389. doi: 10.24875/ACM.21000301.
- Brock R. Functional obstruction of the left ventricle; acquired aortic subvalvar stenosis. Guys Hosp Rep. 1957;106:221-38.
- Teare D. Asymmetrical hypertrophy of the heart in young adults. Br Heart J. 1958 Jan;20(1):1-8. doi: 10.1136/hrt.20.1.1.
- Braunwald E, Lambrew CT, Rockoff SD, Ross J, Morrow AG. Idiopathic hypertrophic subaortic stenosis. I. A description of the disease based upon an analysis of 64 patients. Circulation. 1964 Nov;30:Suppl 4:3-119. doi: 10.1161/01.cir.29.5s4.iv-3.
- Cohen J, Effat H, Goodwin JF, Oakley CM, Steiner RE. Hypertrophic obstructive cardiomyopathy Br Heart J. 1964 Jan;26(1):16-32. doi: 10.1136/hrt.26.1.16.
- Arbustini E, Narula N, Dec G, Reddy K, Greenberg B, Kushwaha S, et al. The MOGE(S) classification for a phenotype-genotype nomenclature of cardiomyopathy. Endorsed by the World Heart Federation. J Am Coll Cardiol. 2013 Dec 3;62(22):2046-72. doi: 10.1016/j.jacc.2013.08.1644.
- Arbustini E, Narula N, Tavazzi L, Serio A, Grasso M, Favalli V, et al. The MOGE(S) classification of cardiomyopathy for clinicians. J Am Coll Cardiol. 2014 Jul 22;64(3):304-18. doi: 10.1016/j.jacc.2014.05.027.
- Arbelo E, Protonotarios A, Gimeno JR, Arbustini E, Barriales-Villa R, Basso C, et al. 2023 ESC Guidelines for the management of cardiomyopathies Developed by the task force on the management of cardiomyopathies of the European Society of Cardiology (ESC). European Heart Journal. 2023 Oct1; 44, (Iss 37):3503-3626. https://doi.org/10.1093/eurheartj/ehad194.
- Pinto YM, Elliott PM, Arbustini E, Adler Y, Anastasakis A, Böhm M, et al. Proposal for a revised definition of dilated cardiomyopathy, hypokinetic non-dilated cardiomyopathy, and its implications for clinical practice: a position statement of the ESC working group on myocardial and pericardial diseases. Eur Heart J. 2016 Jun 14;37(23):1850-8. doi: 10.1093/eurheartj/ehv727.
- Lauer RM, Fink HP, Petry EL, Dunn MI, Diehl AM. Angiographic Demonstration of Intramyocardial Sinusoids in Pulmonary-Valve Atresia with Intact Ventricular Septum and Hypoplastic Right Ventricle. N Engl J Med. 1964 Jul 9;271:68-72. doi: 10.1056/NEJM196407092710203.
- Blixenkrone-Møller E, Dannesbo S, Dehn AM, Pihl CA, Sillesen AS, Vøgg ROB, Raja AA, et al. Prevalence of Left Ventricular Noncompaction in Newborns. Pediatr Cardiol. 2024 Jul 13. doi: 10.1007/s00246-024-03571-0.
- Feldt RH, Rahimtoola SH, Davis GD, Swan H, Titus JL. Anomalous ventricular myocardial patterns in a child with complex congenital heart disease. Am J Cardiol. 1969 May;23(5):732-4. doi: 10.1016/0002-9149(69)90037-x.
- Chin TK, Perloff JK, Williams RG, Jue K, Mohrmann R. Isolated noncompaction of left ventricular myocardium. A study of eight cases. Circulation. 1990 Aug;82(2):507-13. doi: 10.1161/01.cir.82.2.507.
- Ritte M, Oeshlin E, Sutch G, et al. Isolated non-compaction of the myocardium in adults. Mayo Clin. Proct. 1997;72:26-31. https://doi.org/10.4065/72.1.26.
- Dote K, Sato H, Tateishi H, Uchida T, Ishihara M. Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. J Cardiol. 1991;21:203-214.
- Desmet WJ, Adriaenssens BF, Dens JA. Apical ballooning of the left ventricle: first series in white patients. Heart. 2003 Sep;89(9):1027-31. doi: 10.1136/heart.89.9.1027.
- Palmieri G, D’Ambrosio MF, Correale M, Brunetti ND, Santacroce R, Iacoviello M, et al. The Role of Genetics in the Management of Heart Failure Patients. Int J Mol Sci. 2023 Oct 16;24(20):15221. doi: 10.3390/ijms242015221.
- Aiyer S, Kalutskaya E, Agdamag AC, Tang WHW. Genetic Evaluation and Screening in Cardiomyopathies: Opportunities and Challenges for Personalized Medicine. J Pers Med. 2023 May 24;13(6):887. doi: 10.3390/jpm13060887.
- Kontorovich AR. Approaches to Genetic Screening in Cardiomyopathies: Practical Guidance for Clinicians. JACC Heart Fail. 2023. Feb;11(2):133-142. doi: 10.1016/j.jchf.2022.11.025.
- Duarte CW, Vaughan LK, Beasley TM, Tiwari HK. Multifactorial Inheritance and Complex Diseases. Emery and Rimoin’s Principles and Practice of Medical Genetics. 2013;1:1-15. https://doi.org/10.1016/b978-0-12-383834-6.00014-8.
- Mukhopadhyay S, Dixit P, Khanom N, Sanghera G, McGurk KA. The Genetic Factors Influencing Cardiomyopathies and Heart Failure across the Allele Frequency Spectrum. J. of Cardiovasc. Trans. Res. 2024. https://doi.org/10.1007/s12265-024-10520-y.
- McGurk KA, Qiao M, Zheng SL, Sau A, Henry A, Ribeir AL, et al. Genetic and phenotypic architecture of human myocardial trabeculation. MedRxiv. 2024. doi: 10.1101/2024.03.26.24304726.
- Lipov A, Jurgens SJ, Mazzarotto F, Allouba M, Pirruccello JP, Aguib Y, et al. Exploring the complex spectrum of dominance and recessiveness in genetic cardiomyopathies. Nat Cardiovasc Res. 2023;2(11):1078-1094. doi: 10.1038/s44161-023-00346-3.
- Haas J, Frese KS, Peil B, Kloos W, Keller A, Nietsch R, et al. Atlas of the clinical genetics of human dilated cardiomyopathy. Eur Heart J. 2015 May 7;36(18):1123-35. doi: 10.1093/eurheartj/ehu301.
- Watanabe T, Okada H, Kanamori H, Miyazaki N, Tsujimoto A, Takada C, et al. In situ nuclear DNA methylation in dilated cardiomyopathy: an endomyocardial biopsy study. ESC Heart Fail. 2020 Apr;7(2):493-502. doi: 10.1002/ehf2.12593.
- Marian AJ. Sporadic dilated cardiomyopathy is often familial. Cardiovasc Res. 2022 Jul 27;118(10):69-71. doi: 10.1093/cvr/cvac075.
- Sen-Chowdhry S, McKenna WJ. When rare illuminates common: how cardiocutaneous syndromes transformed our perspective on arrhythmogenic cardiomyopathy. Cell Commun Adhes. 2014 Feb;21(1):3-11. doi: 10.3109/15419061.2013.876415.
- Maurer C, Boleti O, Najarzadeh Torbati P, Norouzi F, Fowler ANR, Minaee S, et al. Genetic Insights from Consanguineous Cardiomyopathy Families. Genes (Basel). 2023 Jan 10;14(1):182. doi: 10.3390/genes14010182.
- Luo K, Zheng C, Luo R, Cao X, Sun H, Ma H, et al. Identification and functional characterization of BICD2 as a candidate disease gene in an consanguineous family with dilated cardiomyopathy. BMC Med Genomics. 2022 Sep 6;15(1):189. doi: 10.1186/s12920-022-01349-y.
- Huggins GS, Kinnamon DD, Haas GJ, Jordan E, Hofmeyer M, Kransdorf E, et al. Prevalence and Cumulative Risk of Familial Idiopathic Dilated Cardiomyopathy. JAMA. 2022 Feb 1;327(5):454-463. doi: 10.1001/jama.2021.24674.
- Mallavarapu A, Taksande A. Dilated Cardiomyopathy in Children: Early Detection and Treatment. Cureus. 2022 Nov 4;14(11):e31111. doi: 10.7759/cureus.31111.
- Nannapaneni H, Ghaleb S, Arya S, Gajula V, Taylor MB, Das BB. Further Evidence of Autosomal Recessive Inheritance of RPL3L Pathogenic Variants with Rapidly Progressive Neonatal Dilated Cardiomyopathy. J Cardiovasc Dev Dis. 2022 Feb 22;9(3):65. doi: 10.3390/jcdd9030065.
- Lay E, Azamian MS, Denfield SW, Dreyer W, Spinner JA, Kearney D, et al. LMOD2-related dilated cardiomyopathy presenting in late infancy. Am J Med Genet A. 2022 Jun;188(6):1858-1862. doi: 10.1002/ajmg.a.62699.
- Fragola P, Autore C, Picelli A, Sommariva L, Cannata D, Sangiorgi M. Familial idiopathic dilated cardiomyopathy. Am Heart J. 1988 Apr;115(4):912-4. doi: 10.1016/0002-8703(88)90900-3.
- MacLennan BA, Tsoi EY, Maguire C, Adgey AA. Familial idiopathic congestive cardiomyopathy in three generations: a family study with eight affected members. Q J Med. 1987 Apr;63(240):335-47.
- Gardner RJ, Hanson JW, Ionasescu VV, Ardinger HH, Skorton DJ, Mahoney LT, et al. Dominantly inherited dilated cardiomyopathy. Am J Med Genet. 1987 May;27(1):61-73. doi: 10.1002/ajmg.1320270108.
- Graber HL, Unverferth DV, Baker PB, Ryan JM, Baba N, Wooley CF. Evolution of a hereditary cardiac conduction and muscle disorder: a study involving a family with six generations affected. Circulation. 1986 Jul;74(1):21-35. doi: 10.1161/01.cir.74.1.21.
- Coughlin SS, Szklo M, Baughman K, Pearson TA. The epidemiology of idiopathic dilated cardiomyopathy in a biracial community. Am J Epidemiol. 1990 Jan;131(1):48-56. doi: 10.1093/oxfordjournals.aje.a115484.
- Ozick H, Hollander G, Greengart A, Shani J, Lichstein E. Dilated cardiomyopathy in identical twins. Chest. 1984 Dec;86(6):878-80. doi: 10.1378/chest.86.6.878.
- Lee E, Park KT, Kang J, Park H, Park JJ, Oh IY, et al. A novel c.563 T>G, p.L189R lamin A/C mutation in identical twins with dilated cardiomyopathy. Korean J Intern Med. 2017 Jan;32(1):178-181. doi: 10.3904/kjim.2015.146.
- Walsh R, Offerhaus JA, Tadros R, Bezzina CR. Minor hypertrophic cardiomyopathy genes, major insights into the genetics of cardiomyopathies. Nat Rev Cardiol. 2022 Mar;19(3):151-167 doi: 10.1038/s41569-021-00608-2.
- Pare J, Fraser R, Pirozynski W, Shanks J, Stubington D. Hereditary cardiovascular dysplasia. A form of familial cardiomyopathy. Am J Med. 1961 Jul;31:37-62. doi: 10.1016/0002-9343(61)90222-4.
- Clark CE, Henry WL, Epstein SE. Familial prevalence and genetic transmission of idiopathic hypertrophic subaortic stenosis. N Engl J Med. 1973 Oct 4;289(14):709-14. doi: 10.1056/NEJM197310042891402.
- Maron BJ, Henry WL, Clark CE, Redwood DR, Roberts WC, Epstein SE. Asymetric septal hypertrophy in childhood. Circulation. 1976 Jan;53(1):9-19. doi: 10.1161/01.cir.53.1.9.
- Greaves SC, Roche AH, Neutze JM, Whitlock RM, Veale AM. Inheritance of hypertrophic cardiomyopathy: a cross sectional and M mode echocardiographic study of 50 families. Br Heart J. 1987 Sep;58(3):259-66. doi: 10.1136/hrt.58.3.259.
- Erdmann J, Daehmlow S, Wischke S, Senyuva M, Werner U, Raible J, et al. Mutation spectrum in a large cohort of unrelated consecutive patients with hypertrophic cardiomyopathy. Clin Genet. 2003 Oct;64(4):339-49. doi: 10.1034/j.1399-0004.2003.00151.x.
- Ingles J, Doolan A, Chiu C, Seidman J, Seidman C, Semsarian C. Compound and double mutations in patients with hypertrophic cardiomyopathy: implications for genetic testing and counselling. J Med Genet. 2005 Oct;42(10):59. doi: 10.1136/jmg.2005.033886.
- Ingles J, Sarina T, Yeates L, Hunt L, Macciocca I, McCormack L, et al. Clinical predictors of genetic testing outcomes in hypertrophic cardiomyopathy. Genet Med. 2013 Dec;15(12):972-7. doi: 10.1038/gim.2013.44.
- Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009 Mar 3;119(8):1085-92. doi: 10.1161/CIRCULATIONAHA.108.804617.
- Cannon RO 3rd. Assessing risk in hypertrophic cardiomyopathy. N Engl J Med. 2003 Sep 11;349(11):1016-8. doi: 10.1056/NEJMp038122.
- Watkins H, Rosenzweig A, Hwang DS, Levi T, McKenna W, Seidman CE, et al. Characteristics and prognostic implications of myosin missense mutations in familial hypertrophic cardiomyopathy. N Engl J Med. 1992 Apr 23;326(17):1108-14. doi: 10.1056/NEJM199204233261703.
- Ditaranto R, Caponetti AG, Ferrara V, Parisi V, Minnucci M, Chiti C, et al. Pediatric Restrictive Cardiomyopathies. Front Pediatr. 2022 Jan 25;9:745365. doi: 10.3389/fped.2021.745365.
- Anderson HN, Cetta F, Driscoll DJ, Olson TM, Ackerman MJ, Johnson JN. Idiopathic Restrictive Cardiomyopathy in Children and Young Adults. Am J Cardiol. 2018 May 15;121(10):1266-1270. doi: 10.1016/j.amjcard.2018.01.045.
- Fitzpatrick AP, Shapiro LM, Rickards AF, Poole-Wilson PA. Familial restrictive cardiomyopathy with atrioventricular block and skeletal myopathy. Br Heart J. 1990 Feb;63(2):114-8. doi: 10.1136/hrt.63.2.114.
- Katritsis D, Wilmshurst PT, Wendon JA, Davies MJ, Webb-Peploe MM. Primary restrictive cardiomyopathy: clinical and pathologic characteristics. J Am Coll Cardiol. 1991 Nov 1;18(5):1230-5. doi: 10.1016/0735-1097(91)90540-p. PMID: 1918700.
- Ishiwata S, Nishiyama S, Seki A, Kojima S. Restrictive cardiomyopathy with complete atrioventricular block and distal myopathy with rimmed vacuoles. Jpn Circ J. 1993 Sep;57(9):928-33. doi: 10.1253/jcj.57.928.
- Chen SC, Balfour IC, Jureidini S. Clinical spectrum of restrictive cardiomyopathy in children. J Heart Lung Transplant. 2001 Jan;20(1):90-2. doi: 10.1016/s1053-2498(00)00162-5.
- Lorenzo M, Lynch A, Ashkanase J, Fazari L, George K, Arathoon K, et al. Symptomatic presentation influences outcomes in pediatric restrictive cardiomyopathy. Front Pediatr. 2023 Oct 19;11:1264751. doi: 10.3389/fped.2023.1264751.
- Rampazzo A, Nava A, Danieli GA, Buja G, Daliento L, Fasoli G, et al. The gene for arrhythmogenic right ventricular cardiomyopathy maps to chromosome 14q23-q24. Hum Mol Genet. 1994 Jun;3(6):959-62. doi: 10.1093/hmg/3.6.959.
- Beffagna G, Occhi G, Nava A, Vitiello L, Ditadi A, Basso C, et al. Regulatory mutations in transforming growth factor-beta3 gene cause arrhythmogenic right ventricular cardiomyopathy type 1. Cardiovasc Res. 2005 Feb 1;65(2):366-73. doi: 10.1016/j.cardiores.2004.10.005.
- Ohno S. The genetic background of arrhythmogenic right ventricular cardiomyopathy. J Arrhythm. 2016 Oct;32(5):398-403. doi: 10.1016/j.joa.2016.01.006.
- Christensen AH, Benn M, Bundgaard H, Tybjaerg-Hansen A, Haunso S, Svendsen JH. Wide spectrum of desmosomal mutations in Danish patients with arrhythmogenic right ventricular cardiomyopathy. J Med Genet. 2010 Nov;47(11):736-44. doi: 10.1136/jmg.2010.077891.
- Te Riele ASJM, James CA, Calkins H, Tsatsopoulou A. Arrhythmogenic Right Ventricular Cardiomyopathy in Pediatric Patients: An Important but Underrecognized Clinical Entity. Front Pediatr. 2021 Dec 2;9:750916. doi: 10.3389/fped.2021.750916.