Журнал «Медицина неотложных состояний» Том 21, №1, 2025
Вернуться к номеру
Циротична кардіоміопатія як проблема при трансплантації печінки
Авторы: Чуклін С.М., Чуклін С.С.
Медичний центр Святої Параскеви, м. Львів, Україна
Рубрики: Медицина неотложных состояний
Разделы: Справочник специалиста
Версия для печати
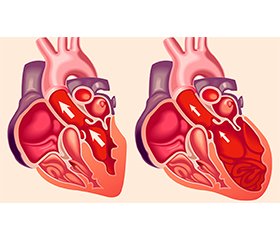
Цироз печінки є важливою причиною смертності, а доступ до трансплантації печінки значно поліпшив його прогноз. Проте більшість пацієнтів у листі очікування на трансплантацію печінки мають термінальну стадію захворювання печінки. Через помітну периферичну вазодилатацію термінальної стадії цирозу, яка маскує приховану дисфункцію міокарда, серцеві аномалії в стані спокою, як правило, є субклінічними, і лікарі не звертають на них уваги. Однак при стресі систолічна та діастолічна функції послаблюються. На додаток до цих аномалій скорочення, можуть спостерігатися морфологічні зміни, як-от збільшення або гіпертрофія серцевих камер, а також електрофізіологічні зміни реполяризації, включно з подовженням інтервалу QT. Сукупність цих серцевих аномалій називається циротичною кардіоміопатією. Трансплантація печінки викликає значний серцево-судинний стрес. Перетискання нижньої порожнистої та ворітної вен, кровотеча та інфузійна терапія, ішемія/реперфузія — все це спричиняє гемодинамічні коливання. Це збільшує робоче навантаження на серце, і, таким чином, раніше субклінічна дисфункція шлуночків може проявлятися у вигляді явної серцевої недостатності під час операційного та післяопераційного періодів. Однак, оскільки трансплантація печінки є єдиним остаточним методом лікування кінцевої стадії печінкової недостатності, а також, ймовірно, усуває кардіоміопатію, важливо розуміти зміни у серцево-судинній системі під час цієї операції. Хоча дані свідчать про те, що циротична кардіоміопатія може бути оборотною після ортотопічної трансплантації, потрібні подальші дослідження цього стану. Цей огляд присвячений фокусуванню на циротичній кардіоміопатії до, під час і після трансплантації печінки. У базах даних MedLine, Scopus було проведено пошук публікацій до 2024 року.
Liver cirrhosis is an important cause of mortality, and access to liver transplantation has significantly improved its prognosis. However, most patients in the liver transplant waiting list have end-stage liver disease. Due to the marked peripheral vasodilatation in end-stage cirrhosis that masks a latent myocardial dysfunction, cardiac abnormalities at rest are usually subclinical and escape the attention of physicians. However, when challenged, the systolic and diastolic functions are attenuated. In addition to these contractile abnormalities, morphological changes can be observed such as cardiac chamber enlargement or hypertrophy, and changes in electrophysiological repolarization, including a prolonged QT interval. A combination of these cardiac abnormalities is termed cirrhotic cardiomyopathy. Liver transplantation induces significant cardiovascular stress. Clamping of the inferior vena cava and portal vein, hemorrhage and infusion therapy, and ischemia/reperfusion all cause hemodynamic fluctuation. This increases the cardiac workload, and thus, subclinical ventricular dysfunction may manifest earlier as overt heart failure during surgery and in the postoperative period. However, because liver transplantation is the only definitive treatment for end-stage liver failure and also appears to reverse cardiomyopathy, it is important to understand the changes in the cardiovascular system during this intervention. Although evidence suggests that cirrhotic cardiomyopathy may be reversible after orthotopic liver transplantation, further investigation is needed. This review focuses on cirrhotic cardiomyopathy before, during, and after liver transplantation. MedLine, Scopus databases were searched for publications up to 2024.
цироз печінки; кардіоміопатія; трансплантація печінки; огляд
liver cirrhosis; cardiomyopathy; liver transplantation; review
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Kaur H, Premkumar M. Diagnosis and Management of Cirrho–tic Cardiomyopathy. J Clin Exp Hepatol. 2022 Jan-Feb;12(1):186-199. doi: 10.1016/j.jceh.2021.08.016.
- Brankovic M, Lee P, Pyrsopoulos N, Klapholz M. Cardiac Syndromes in Liver Disease: A Clinical Conundrum. J Clin Transl Hepatol. 2023 Aug 28;11(4):975-986. doi: 10.14218/JCTH.2022.00294.
- Izzy M, VanWagner LB, Lin G, Altieri M, Findlay JY, Oh JK, et al. Redefining Cirrhotic Cardiomyopathy for the Modern Era. Hepatology. 2020 Jan;71(1):334-345. doi: 10.1002/hep.30875.
- Kalluru R, Gadde S, Chikatmalla R, Dasaradhan T, Koneti J, Cherukuri SP. Cirrhotic Cardiomyopathy: The Interplay Between Liver and Heart. Cureus. 2022 Aug 13;14(8):e27969. doi: 10.7759/cureus.27969.
- Yoon KT, Liu H, Lee SS. Cirrhotic Cardiomyopathy. Curr Gastroenterol Rep. 2020 Jul 10;22(9):45. doi: 10.1007/s11894-020-00783-1.
- Zardi EM, Zardi DM, Chin D, Sonnino C, Dobrina A, Abbate A. Cirrhotic cardiomyopathy in the pre- and post-liver transplantation phase. J Cardiol. 2016 Feb;67(2):125-30. doi: 10.1016/j.jjcc.2015.04.016.
- Liu H, Jayakumar S, Traboulsi M, Lee SS. Cirrhotic cardiomyopathy: Implications for liver transplantation. Liver Transpl. 2017 Jun;23(6):826-835. doi: 10.1002/lt.24768.
- Møller S, Danielsen KV, Wiese S, Hove JD, Bendtsen F. An update on cirrhotic cardiomyopathy. Expert Rev Gastroenterol Hepatol. 2019 May;13(5):497-505. doi: 10.1080/17474124.2019.1587293.
- Izzy M, Soldatova A, Sun X, Angirekula M, Mara K, Lin G, et al. Cirrhotic Cardiomyopathy Predicts Posttransplant Cardiovascular Disease: Revelations of the New Diagnostic Criteria. Liver Transpl. 2021 Jun;27(6):876-886. doi: 10.1002/lt.26000.
- Sonny A, Ibrahim A, Schuster A, Jaber WA, Cywinski JB. Impact and persistence of cirrhotic cardiomyopathy after liver transplantation. Clin Transplant. 2016 Sep;30(9):986-93. doi: 10.1111/ctr.12778.
- Izzy M, Oh J, Watt KD. Cirrhotic Cardiomyopathy After Transplantation: Neither the Transient Nor Innocent Bystander. Hepatology. 2018 Nov;68(5):2008-2015. doi: 10.1002/hep.30040.
- Koshy AN, Gow PJ, Han HC, Teh AW, Jones R, Testro A, et al. Cardiovascular mortality following liver transplantation: predictors and temporal trends over 30 years. Eur Heart J Qual Care Clin Outcomes. 2020 Oct 1;6(4):243-253. doi: 10.1093/ehjqcco/qcaa009.
- VanWagner LB, Ning H, Whitsett M, Levitsky J, Uttal S, Wilkins JT, et al. A point-based prediction model for cardiovascular risk in orthotopic liver transplantation: The CAR-OLT score. Hepato-logy. 2017 Dec;66(6):1968-1979. doi: 10.1002/hep.29329.
- Altayar O, Lisker-Melman M. Physiologic Adaptation or Cirrhotic Cardiomyopathy: It Is Time for New Definitions! J Card Fail. 2019 Mar;25(3):173-175. doi: 10.1016/j.cardfail.2019.01.013.
- Karagiannakis DS, Vlachogiannakos J, Anastasiadis G, Vafiadis-Zouboulis I, Ladas SD. Diastolic cardiac dysfunction is a predictor of dismal prognosis in patients with liver cirrhosis. Hepatol Int. 2014 Oct;8(4):588-94. doi: 10.1007/s12072-014-9544-6.
- Ruíz-del-Árbol L, Achécar L, Serradilla R, Rodríguez-Gandía MÁ, Rivero M, Garrido E, et al. Diastolic dysfunction is a predictor of poor outcomes in patients with cirrhosis, portal hypertension, and a normal creatinine. Hepatology. 2013 Nov;58(5):1732-41. doi: 10.1002/hep.26509.
- Mittal C, Qureshi W, Singla S, Ahmad U, Huang MA. Pre-transplant left ventricular diastolic dysfunction is associated with post transplant acute graft rejection and graft failure. Dig Dis Sci. 2014 Mar;59(3):674-80. doi: 10.1007/s10620-013-2955-8.
- Darstein F, König C, Hoppe-Lotichius M, Grimm D, Knapstein J, Mittler J, et al. Preoperative left ventricular hypertrophy is associated with reduced patient survival after liver transplantation. Clin Transplant. 2014 Feb;28(2):236-42. doi: 10.1111/ctr.12304.
- Sonny A, Govindarajan SR, Jaber WA, Cywinski JB. Systolic heart failure after liver transplantation: Incidence, predictors, and outcome. Clin Transplant. 2018 Mar;32(3):e13199. doi: 10.1111/ctr.13199.
- Sharma S, Prasad A, Karamchandani K. Extracorporeal Membrane Oxygenation in a Patient With Cirrhotic Cardiomyopathy: A Case Report. J Cardiothorac Vasc Anesth. 2019 Jan;33(1):173-175. doi: 10.1053/j.jvca.2018.02.017.
- Sakr AE, Fraser GE, Doctorian TP, Kim HB, Narasimha D, Abudayyeh I, et al. Predictors of Systolic Heart Failure and Mortality Following Orthotopic Liver Transplantation: a Single-Center Cohort. Transplant Proc. 2019 Jul-Aug;51(6):1950-1955. doi: 10.1016/j.transproceed.2019.04.063.
- Eyvazian VA, Gordin JS, Yang EH, Aksoy O, Honda HM, Busuttil RW, et al. Incidence, Predictors, and Outcomes of New-Onset Left Ventricular Systolic Dysfunction After Orthotopic Liver Transplantation. J Card Fail. 2019 Mar;25(3):166-172. doi: 10.1016/j.cardfail.2018.10.013.
- Gorgis NM, Kennedy C, Lam F, Thompson K, Coss-Bu J, Akcan Arikan A, et al. Clinical Consequences of Cardiomyopathy in Children With Biliary Atresia Requiring Liver Transplantation. Hepatology. 2019 Mar;69(3):1206-1218. doi: 10.1002/hep.30204.
- Baibhav B, Mahabir CA, Xie F, Shostrom VK, McCashland TM, Porter TR. Predictive Value of Dobutamine Stress Perfusion Echocardiography in Contemporary End-Stage Liver Di–sease. J Am Heart Assoc. 2017 Feb 20;6(2):e005102. doi: 10.1161/JAHA.116.005102.
- Aggeli C, Polytarchou K, Varvarousis D, Kastellanos S, Tousoulis D. Stress ECHO beyond coronary artery disease. Is it the holy grail of cardiovascular imaging? Clin Cardiol. 2018 Dec;41(12):1600-1610. doi: 10.1002/clc.23094.
- Lancellotti P, Pellikka PA, Budts W, Chaudhry FA, Donal E, Dulgheru R, et al. The clinical use of stress echocardiography in non-ischemic heart disease: Recommendations from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging. 2016 Nov;17(11):1191-1229. doi: 10.1093/ehjci/jew190.
- Lai JC, Sonnenday CJ, Tapper EB, Duarte-Rojo A, Dunn MA, Bernal W, et al. Frailty in liver transplantation: An expert opinion statement from the American Society of Transplantation Liver and Intestinal Community of Practice. Am J Transplant. 2019 Jul;19(7):1896-1906. doi: 10.1111/ajt.15392.
- Ney M, Haykowsky MJ, Vandermeer B, Shah A, Ow M, Tandon P. Systematic review: pre- and post-operative prognostic value of cardiopulmonary exercise testing in liver transplant candidates. Aliment Pharmacol Ther. 2016 Oct;44(8):796-806. doi: 10.1111/apt.13771.
- Wiese S, Hove J, Mo S, Mookerjee RP, Petersen CL, Vester-Andersen MK, et al. Myocardial extracellular volume quantified by magnetic resonance is increased in cirrhosis and related to poor outcome. Liver Int. 2018 Sep;38(9):1614-1623. doi: 10.1111/liv.13870.
- Dowsley TF, Bayne DB, Langnas AN, Dumitru I, Windle JR, Porter TR, et al. Diastolic dysfunction in patients with end-stage liver disease is associated with development of heart failure early after liver transplantation. Transplantation. 2012 Sep 27;94(6):646-51. doi: 10.1097/TP.0b013e31825f0f97.
- Kim KS, Kwon HM, Jung KW, Sang BH, Moon YJ, Kim B, et al. Markedly prolonged QTc interval in end-stage liver disease and risk of 30-day cardiovascular event after liver transplant. J Gastroenterol Hepatol. 2021 Mar;36(3):758-766. doi: 10.1111/jgh.15179.
- Ko J, Koshy AN, Han HC, Weinberg L, Gow P, Testro A, et al. Effect of liver transplantation on QT-interval prolongation and impact on mortality. Int J Cardiol. 2021 Mar 1;326:158-163. doi: 10.1016/j.ijcard.2020.11.017.
- Huffman C, Wagman G, Fudim M, Zolty R, Vittorio T. Reversible cardiomyopathies — a review. Transplant Proc. 2010 Nov;42(9):3673-8. doi: 10.1016/j.transproceed.2010.08.034.
- Junge N, Junge C, Schröder J, Pfister ED, Leiskau C, Hoh–mann D, et al. Pediatric cirrhotic cardiomyopathy: Impact on liver transplant outcomes. Liver Transpl. 2018 Jun;24(6):820-830. doi: 10.1002/lt.25076.
- Saner FH, Neumann T, Canbay A, Treckmann JW, Hartmann M, Goerlinger K, et al. High brain-natriuretic peptide level predicts cirrhotic cardiomyopathy in liver transplant patients. Transpl Int. 2011 May;24(5):425-32. doi: 10.1111/j.1432-2277.2011.01219.x.
- Ziada D, Gaber R, Kot N, Ghazy M, Nagy H. Predictive Value of N-terminal Pro B-type Natriuretic Peptide in Tissue Doppler-Diagnosed Cirrhotic Cardiomyopathy. Heart Mirror J. 2011;5(1):186-191.
- Qureshi W, Mittal C, Ahmad U, Alirhayim Z, Hassan S, Qureshi S, et al. Clinical predictors of post-liver transplant new-onset heart failure. Liver Transpl. 2013 Jul;19(7):701-10. doi: 10.1002/lt.23654.
- Bernal V, Pascual I, Lanas A, Esquivias P, Piazuelo E, Garcia-Gil FA, et al. Cardiac function and aminoterminal pro-brain natriuretic peptide levels in liver-transplanted cirrhotic patients. Clin Transplant. 2012 Jan-Feb;26(1):111-6. doi: 10.1111/j.1399-0012.2011.01438.x.
- Toussaint A, Weiss E, Khoy-Ear L, Janny S, Cohen J, Delefosse D, et al. Prognostic Value of Preoperative Brain Natriuretic Peptide Serum Levels in Liver Transplantation. Transplantation. 2016 Apr;100(4):819-24. doi: 10.1097/TP.0000000000001077.
- Park J, Lee SH, Han S, Jee HS, Lee SK, Choi GS, et al. Preoperative cardiac troponin level is associated with all-cause mortality of liver transplantation recipients. PLoS One. 2017 May 23;12(5):e0177838. doi: 10.1371/journal.pone.0177838.
- Główczyńska R, Raszeja-Wyszomirska J, Janik M, Kostrzewa K, Zygmunt M, Zborowska H, et al. Troponin I Is Not a Predictor of Early Cardiovascular Morbidity in Liver Transplant Recipients. Transplant Proc. 2018 Sep;50(7):2022-2026. doi: 10.1016/j.transproceed.2018.02.136.
- Watt KD, Coss E, Pedersen RA, Dierkhising R, Heimbach JK, Charlton MR. Pretransplant serum troponin levels are highly predictive of patient and graft survival following liver transplantation. Liver Transpl. 2010 Aug;16(8):990-8. doi: 10.1002/lt.22102.
- Moon YJ, Kwon HM, Jung KW, Kim KS, Shin WJ, Jun IG, et al. Preoperative high-sensitivity troponin I and B-type natriuretic peptide, alone and in combination, for risk stratification of mortality after liver transplantation. Korean J Anesthesiol. 2021 Jun;74(3):242-253. doi: 10.4097/kja.20296.
- Vilchez-Monge AL, Garutti I, Jimeno C, Zaballos M, Jimenez C, Olmedilla L, et al. Intraoperative Troponin Elevation in Liver Transplantation Is Independently Associated With Mortality: A Prospective Observational Study. Liver Transpl. 2020 May;26(5):681-692. doi: 10.1002/lt.25716.
- Park J, Lee SH, Han S, Kim KY, Kim GE, Park M, et al. Elevated High-Sensitivity Troponin I During Living Donor Liver Transplantation Is Associated With Postoperative Adverse Outcomes. Transplantation. 2018 May;102(5):e236-e244. doi: 10.1097/TP.0000000000002068.
- Jankowski K, Trzebicki J, Bielecki M, Łągiewska B, Kurnicka K, Koczaj-Bremer M, et al. Prognostic value of perioperative assessment of plasma cardiac troponin I in patients undergoing liver transplantation. Acta Biochim Pol. 2017;64(2):331-337. doi: 10.18388/abp.2016_1436.
- Siniscalchi A, Gamberini L, Mordenti A, Bernardi E, Cimatti M, Riganello I, et al. Postoperative troponin T elevation as a predictor of early acute kidney injury after orthotopic liver transplantation: a preliminary retrospective study. Transplant Proc. 2012 Sep;44(7):1999-2001. doi: 10.1016/j.transproceed.2012.06.039.
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018 Aug;69(2):406-460. doi: 10.1016/j.jhep.2018.03.024.
- Harinstein ME, Iyer S, Mathier MA, Flaherty JD, Fontes P, Planinsic RM, et al. Role of baseline echocardiography in the preoperative management of liver transplant candidates. Am J Cardiol. 2012 Dec 15;110(12):1852-5. doi: 10.1016/j.amjcard.2012.08.021.
- Isaak A, Praktiknjo M, Jansen C, Faron A, Sprinkart AM, Pieper CC, et al. Myocardial Fibrosis and Inflammation in Li-
- ver Cirrhosis: MRI Study of the Liver-Heart Axis. Radiology. 2020 Oct;297(1):51-61. doi: 10.1148/radiol.2020201057.
- Raval Z, Harinstein ME, Flaherty JD. Role of cardiovascular intervention as a bridge to liver transplantation. World J Gastroenterol. 2014 Aug 21;20(31):10651-7. doi: 10.3748/wjg.v20.i31.10651.
- Patel S, Siddiqui MB, Chandrakumaran A, Rodriguez VA, Faridnia M, Hernandez Roman J, et al. Progression to Cirrhosis Leads to Improvement in Atherogenic Milieu. Dig Dis Sci. 2021 Jan;66(1):263-272. doi: 10.1007/s10620-020-06196-4.
- Shroff H, Rinella ME. Thanks to CLD for Small Favors: Reduced CVD Risk in Patients Awaiting Liver Transplantation. Dig Dis Sci. 2021 Jan;66(1):7-9. doi: 10.1007/s10620-020-06322-2.
- De Pietri L, Mocchegiani F, Leuzzi C, Montalti R, Viva-relli M, Agnoletti V. Transoesophageal echocardiography during liver transplantation. World J Hepatol. 2015 Oct 18;7(23):2432-48. doi: 10.4254/wjh.v7.i23.2432.
- Siniscalchi A, Gamberini L, Laici C, Bardi T, Ercolani G, Lorenzini L, et al. Post reperfusion syndrome during liver transplantation: From pathophysiology to therapy and preventive strategies. World J Gastroenterol. 2016 Jan 28;22(4):1551-69. doi: 10.3748/wjg.v22.i4.1551.
- Elleuch N, Mrabet S, Ben Slama A, Jaziri H, Hammami A, Brahim A, et al. Cirrhotic cardiomyopathy. Tunis Med. 2020 Mar;98(3):206-210. PMID: 32395813.
- Ruiz-del-Árbol L, Serradilla R. Cirrhotic cardiomyopathy. World J Gastroenterol. 2015 Nov 7;21(41):11502-21. doi: 10.3748/wjg.v21.i41.11502.
- Ripoll C, Yotti R, Bermejo J, Bañares R. The heart in liver transplantation. J Hepatol. 2011 Apr;54(4):810-22. doi: 10.1016/j.jhep.2010.11.003.
- Della Rocca G, Costa MG, Pompei L, Chiarandini P. The liver transplant recipient with cardiac disease. Transplant Proc. 2008 May;40(4):1172-4. doi: 10.1016/j.transproceed.2008.03.070.
- Han S, Park J, Hong SH, Park CS, Choi J, Chae MS. Cardiovascular manifestation of end-stage liver disease and perioperative echocardiography for liver transplantation: anesthesiologist's view. Anesth Pain Med (Seoul). 2022 Apr;17(2):132-144. doi: 10.17085/apm.22132.
- Kim HM, Kim HK, Lee JH, Lee YB, Park EA, Park JB, et al. Myocardial structural and functional changes in patients with liver cirrhosis awaiting liver transplantation: a comprehensive cardiovascular magnetic resonance and echocardiographic study. J Cardiovasc Magn Reson. 2020 Apr 23;22(1):25. doi: 10.1186/s12968-020-00622-2.
- Chahal D, Liu H, Shamatutu C, Sidhu H, Lee SS, Marquez V. Review article: comprehensive analysis of cirrhotic cardiomyopathy. Aliment Pharmacol Ther. 2021 May;53(9):985-998. doi: 10.1111/apt.16305.
- Rahman S, Mallett SV. Cirrhotic cardiomyopathy: Implications for the perioperative management of liver transplant patients. World J Hepatol. 2015 Mar 27;7(3):507-20. doi: 10.4254/wjh.v7.i3.507.
- Torregrosa M, Aguadé S, Dos L, Segura R, Gónzalez A, Evangelista A, et al. Cardiac alterations in cirrhosis: reversibility after liver transplantation. J Hepatol. 2005 Jan;42(1):68-74. doi: 10.1016/j.jhep.2004.09.008.
- Gajanana D, Gupta S, Koshkelashvili N, Rubio M, Bhalla V, Amanullah A. Electrocardiographic and echocardiographic changes in patients undergoing liver transplant stratified by outcomes. Int J Cardiol. 2016 Nov 15;223:699-700. doi: 10.1016/j.ijcard.2016.08.056.
- Khemakanok K, Khositseth A, Treepongkaruna S, Teera-ratkul S, Pansrimangkorn W, Leelaudomlipi S, et al. Cardiac abnormalities in cirrhotic children: pre- and post-liver transplantation. Hepatol Int. 2016 May;10(3):518-24. doi: 10.1007/s12072-015-9674-5.
- Chen Y, Chan AC, Chan SC, Chok SH, Sharr W, Fung J, et al. A detailed evaluation of cardiac function in cirrhotic patients and its alteration with or without liver transplantation. J Cardiol. 2016 Feb;67(2):140-6. doi: 10.1016/j.jjcc.2015.08.001.
- Acosta F, De La Morena G, Villegas M, Sansano T, Reche M, Beltran R, et al. Evaluation of cardiac function before and after li-ver transplantation. Transplant Proc. 1999 Sep;31(6):2369-70. doi: 10.1016/s0041-1345(99)00383-8.
- Karagiannakis DS, Papatheodoridis G, Vlachogiannakos J. Recent advances in cirrhotic cardiomyopathy. Dig Dis Sci. 2015 May;60(5):1141-51. doi: 10.1007/s10620-014-3432-8.
- Glowczynska R, Galas M, Ołdakowska-Jedynak U, Peller M, Tomaniak M, Raszeja-Wyszomirska J, et al. Pretransplant QT Interval: The Relationship with Severity and Etiology of Liver Disease and Prognostic Value After Liver Transplantation. Ann Transplant. 2018 Sep 4;23:622-630. doi: 10.12659/AOT.908769.