Журнал "Гастроэнтерология" Том 59, №1, 2025
Вернуться к номеру
Посттрансляційні модифікації гістонів, що асоційовані з розвитком метаболічно асоційованої жирової хвороби печінки. Частина 3. Ацетилювання гістонів
Авторы: Абатуров О.Є., Нікуліна А.О.
Дніпровський державний медичний університет, м. Дніпро, Україна
Рубрики: Гастроэнтерология
Разделы: Справочник специалиста
Версия для печати
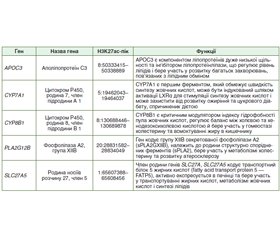
На основі аналізу літературних джерел бази даних Pubmed, MedLine, The Cochrane Library, EMBASE автори статті наводять загальні положення стосовно ацетилювання гістонів. Автори акцентують увагу, що саме ацетилювання лізинового залишку є ключовою посттрансляційною модифікацією гістонів епігенетичними механізмами регуляції експресії генів. На сьогодні ідентифіковано не менше ніж 2000 білків людини, які можуть бути модифіковані за залишками лізину за допомогою ацетилювання. Близько 1000 білків у тканині печінки людини піддаються модифікації ацетилюванням лізину. Ацетилювання опосередковується гістоновими ацетилтрансферазами (histone acetyl transferases — HAT/KAT) і зазвичай пов’язане з активною транскрипцією гена через його здатність деконденсувати хроматин. Навпаки, гістонові деацетилази (histone deacetylases — HDAC/KDAC) видаляють ацетильну групу з лізинового залишку гістонів і таким чином відновлюють компактну форму хроматину. Стан ацетилювання таргетних сайтів визначається балансом активності між процесами ацетилювання та деацетилювання N-термінальних регіонів молекул гістонів. Гіперацетилювання гістонів може бути обумовлено як підвищенням активності HAT/KAT, так і зниженням експресії HDAC. Гістонові ацетилтрансферази каталізують перенесення ацетильної групи з ацетил-КоА на епсилон-аміногрупу лізину, нейтралізуючи позитивний заряд лізину та послаблюючи взаємодію між гістонами та молекулою ДНК. Ацетилювання гістонів завжди асоційоване з відкриттям хроматину та активацією транскрипції генів. Автори наголошують, що збільшення представництва ацетильованих маркерів пов’язане з прогресуванням метаболічно асоційованої жирової хвороби печінки (МАЖХП). Особливо високий рівень ацетилювання (гіперацетилювання) при розвитку МАЖХП відзначається на сайтах K9, K14 та K18 гістону 3. На сьогодні епігенетичні механізми, що визначають стан ацетилювання гістонів у ділянці певних генів, розглядаються як потенційні мішені для медикаментозного впливу. Вивчення впливу ацетилювання гістонів на морфологічні зміни тканини та розвиток метаболічних розладів є підґрунтям, що дозволить розробити ефективні епігенетичні методи лікування хворих на МАЖХП.
Based on the analysis of literature sources from the Pubmed, MEDLINE, The Cochrane Library, Embase databases, the authors of the article highlight general provisions regarding histone acetylation. They emphasize that it is acetylation of the lysine residue that is the key post-translational modification of histones by epigenetic mechanisms of gene expression regulation. To date, at least 2000 human proteins have been identified that can be modified at lysine residues by acetylation. About 1000 proteins in human liver tissue undergo modification by lysine acetylation. Acetylation is mediated by histone acetyltransferases (HAT/KAT) and is usually associated with active gene transcription due to its ability to decondense chromatin. In contrast, histone deacetylases (HDAC/KDAC) remove the acetyl group from the lysine residue of histones and, thus, restore the compact form of chromatin. The acetylation state of target sites is determined by the balance of activity between the processes of acetylation and deacetylation of the N-terminal regions of histone molecules. Histone hyperacetylation can be caused by both increased HAT/KAT activity and decreased HDAC expression. Histone acetyltransferases catalyze the transfer of an acetyl group from acetyl-CoA to the epsilon-amino group of lysine, neutralizing the positive charge of lysine and weakening the interaction between histones and the DNA molecule. Histone acetylation is always associated with chromatin opening and activation of gene transcription. The authors emphasize that an increase in the representation of acetylated markers is associated with the progression of metabolic dysfunction-associated fatty liver disease (MAFLD). A particularly high level of acetylation (hyperacetylation) in MAFLD is noted at sites K9, K14 and K18 of histone 3. Today, epigenetic mechanisms that determine the state of histone acetylation in the region of certain genes are considered as potential targets for drug treatment. Studying the influence of histone acetylation on morphological changes in tissue and the development of metabolic disorders is the basis that will allow developing effective epigenetic methods for treatment of patients with MAFLD.
ожиріння; метаболічно асоційована жирова хвороба печінки; ацетилювання гістонів
obesity; metabolic dysfunction-associated fatty liver disease; histone acetylation
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Eslam M., Newsome P.N., Sarin S.K., et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020 Jul;73(1):202-209. doi: 10.1016/j.jhep.2020.03.039. Epub 2020 Apr 8. PMID: 32278004.
- Tang S.Y., Tan J.S., Pang X.Z., et al. Metabolic dysfunction associated fatty liver disease: The new nomenclature and its impact. World J Gastroenterol. 2023 Jan 21;29(3):549-560. doi: 10.3748/wjg.v29.i3.549. PMID: 36688021; PMCID: PMC9850940.
- Bawiskar N., Acharya S., Kumar S. Fatty liver disease — non alcoholic to metabolic — A transition of concepts! J Family Med Prim Care. 2024 Aug;13(8):2857-2862. doi: 10.4103/jfmpc.jfmpc_1863_21. Epub 2024 Jul 26. PMID: 39228650; PMCID: PMC11368329.
- Chan K.E., Koh T.J.L., Tang A.S.P., et al. Global Prevalence and Clinical Characteristics of Metabolic-associated Fatty Liver Di–sease: A Meta-Analysis and Systematic Review of 10 739 607 Indivi–duals. J Clin Endocrinol Metab. 2022 Aug 18;107(9):2691-2700. doi: 10.1210/clinem/dgac321. PMID: 35587339.
- Fouad Y., Alboraie M., Shiha G. Epidemiology and diagnosis of metabolic dysfunction-associated fatty liver disease. Hepatol Int. 2024 Oct;18(Suppl 2):827-833. doi: 10.1007/s12072-024-10704-3. Epub 2024 Jul 5. PMID: 38967907; PMCID: PMC11450050.
- Cai Q., Gan C., Tang C., et al. Mechanism and Therapeutic Opportunities of Histone Modifications in Chronic Liver Disease. Front Pharmacol. 2021 Nov 23;12:784591. doi: 10.3389/fphar.2021.784591. PMID: 34887768; PMCID: PMC8650224.
- Zhu X., Xia M., Gao X. Update on genetics and epigenetics in me–tabolic associated fatty liver disease. Ther Adv Endocrinol Metab. 2022 Oct 28;13:20420188221132138. doi: 10.1177/20420188221132138. PMID: 36325500; PMCID: PMC9619279.
- Shi Y., Qi W. Histone Modifications in NAFLD: Mechanisms and Potential Therapy. Int J Mol Sci. 2023 Sep 27;24(19):14653. doi: 10.3390/ijms241914653. PMID: 37834101; PMCID: PMC10572202.
- Rodríguez-Sanabria J.S., Escutia-Gutiérrez R., Rosas-Campos R., et al. An Update in Epigenetics in Metabolic-Associated Fatty Liver Disease. Front Med (Lausanne). 2022 Jan 11;8:770504. doi: 10.3389/fmed.2021.770504. PMID: 35087844; PMCID: PMC8787199.
- Abaturov O., Nikulina A. Post-translational histone modi–fications associated with the development of metabolically associa–ted fatty liver disease. Part 1. General provisions. Gastroenterologìa. 2024;58(3):210-221. doi.org/10.22141/2308-2097.58.3.2024.626. [Article in Ukrainian].
- Gil J., Ramírez-Torres A., Encarnación-Guevara S. Lysine acetylation and cancer: A proteomics perspective. J Proteomics. 2017 Jan 6;150:297-309. doi: 10.1016/j.jprot.2016.10.003. Epub 2016 Oct 13. PMID: 27746255.
- Zhao S., Xu W., Jiang W., et al. Regulation of cellular metabolism by protein lysine acetylation. Science. 2010 Feb 19;327(5968):1000-4. doi: 10.1126/science.1179689. PMID: 20167786; PMCID: PMC3232675.
- Zhang Y., Zhou F., Bai M., et al. The pivotal role of protein acetylation in linking glucose and fatty acid metabolism to β-cell function. Cell Death Dis. 2019 Jan 25;10(2):66. doi: 10.1038/s41419-019-1349-z. PMID: 30683850; PMCID: PMC6347623.
- Narita T., Weinert B.T., Choudhary C. Functions and mecha–nisms of non-histone protein acetylation. Nat Rev Mol Cell Biol. 2019 Mar;20(3):156-174. doi: 10.1038/s41580-018-0081-3. Erratum in: Nat Rev Mol Cell Biol. 2019 Aug;20(8):508. PMID: 30467427.
- Shvedunova M., Akhtar A. Modulation of cellular processes by histone and non-histone protein acetylation. Nat Rev Mol Cell Biol. 2022 May;23(5):329-349. doi: 10.1038/s41580-021-00441-y. Epub 2022 Jan 18. PMID: 35042977.
- He W., Li Q., Li X. Acetyl-CoA regulates lipid metabolism and histone acetylation modification in cancer. Biochim Biophys Acta Rev Cancer. 2023 Jan;1878(1):188837. doi: 10.1016/j.bbcan.2022.188837. Epub 2022 Nov 17. PMID: 36403921.
- Lee J., Song J.H., Chung M.Y., et al. 3,4-dihydroxytoluene, a metabolite of rutin, suppresses the progression of nonalcoholic fatty liver disease in mice by inhibiting p300 histone acetyltransferase activity. Acta Pharmacol Sin. 2021 Sep;42(9):1449-1460. doi: 10.1038/s41401-020-00571-7. Epub 2020 Dec 10. PMID: 33303988; PMCID: PMC8379200.
- Chung S., Hwang J.T., Park J.H., et al. Free fatty acid-induced histone acetyltransferase activity accelerates lipid accumulation in HepG2 cells. Nutr Res Pract. 2019 Jun;13(3):196-204. doi: 10.4162/nrp.2019.13.3.196. Epub 2019 Apr 12. PMID: 31214287; PMCID: PMC6548710.
- Fu S., Yu M., Tan Y., et al. Role of histone deacetylase on nonalcoholic fatty liver disease. Expert Rev Gastroenterol Hepatol. 2021 Apr;15(4):353-361. doi: 10.1080/17474124.2021.1854089. Epub 2020 Dec 1. PMID: 33213187.
- Liu R., Li Y., Zheng Q., et al. Epigenetic modification in liver fibrosis: Promising therapeutic direction with significant challenges ahead. Acta Pharm Sin B. 2024 Mar;14(3):1009-1029. doi: 10.1016/j.apsb.2023.10.023. Epub 2023 Nov 4. PMID: 38486982; PMCID: PMC10935124.
- Moran-Salvador E., Mann J. Epigenetics and Liver Fibrosis. Cell Mol Gastroenterol Hepatol. 2017 Apr 26;4(1):125-134. doi: 10.1016/j.jcmgh.2017.04.007. PMID: 28593184; PMCID: PMC5453904.
- Claveria-Cabello A., Colyn L., Arechederra M., et al. Epigenetics in Liver Fibrosis: Could HDACs be a Therapeutic Target? Cells. 2020 Oct 19;9(10):2321. doi: 10.3390/cells9102321. PMID: 33086678; PMCID: PMC7589994.
- Alrob O.A., Sankaralingam S., Ma C., et al. Obesity-induced lysine acetylation increases cardiac fatty acid oxidation and impairs insulin signalling. Cardiovasc Res. 2014 Sep 1;103(4):485-97. doi: 10.1093/cvr/cvu156. Epub 2014 Jun 25. PMID: 24966184; PMCID: PMC4155471.
- Guillemette B., Drogaris P., Lin H.H., et al. H3 lysine 4 is acetylated at active gene promoters and is regulated by H3 lysine 4 methylation. PLoS Genet. 2011 Mar;7(3):e1001354. doi: 10.1371/journal.pgen.1001354. Epub 2011 Mar 31. PMID: 21483810; PMCID: PMC3069113.
- Kang Y., Kim Y.W., Kang J., et al. Histone H3K4me1 and H3K27ac play roles in nucleosome eviction and eRNA transcription, respectively, at enhancers. FASEB J. 2021 Aug;35(8):e21781. doi: 10.1096/fj.202100488R. PMID: 34309923.
- Kang J., Kang Y., Kim A. Histone H3K4ac, as a marker of active transcription start sites and enhancers, plays roles in histone eviction and RNA transcription. Biochim Biophys Acta Gene Regul Mech. 2024 Feb 27;1867(2):195021. doi: 10.1016/j.bbagrm.2024.195021. Epub ahead of print. PMID: 38417480.
- Jin J., Iakova P., Breaux M., et al. Increased expression of enzymes of triglyceride synthesis is essential for the development of hepatic steatosis. Cell Rep. 2013 Mar 28;3(3):831-43. doi: 10.1016/j.celrep.2013.02.009. Epub 2013 Mar 14. PMID: 23499441; PMCID: PMC3615099.
- Cai C., Yu H., Huang G., et al. Histone modifications in fatty acid synthase modulated by carbohydrate responsive element binding protein are associated with non‑alcoholic fatty liver disease. Int J Mol Med. 2018 Sep;42(3):1215-1228. doi: 10.3892/ijmm.2018.3702. Epub 2018 May 22. PMID: 29786745; PMCID: PMC6089769.
- Du X., Cai C., Yao J., et al. Histone modifications in FASN mo–dulated by sterol regulatory element-binding protein 1c and carbohydrate responsive-element binding protein under insulin stimulation are related to NAFLD. Biochem Biophys Res Commun. 2017 Jan 29;483(1):409-417. doi: 10.1016/j.bbrc.2016.12.129. Epub 2016 Dec 24. PMID: 28027934.
- Abaturov O.E., Nikulina A.O. Metabolically associated fatty liver disease in children. Dnipro: Lira, 2021. Р. 724. [Ukrainian].
- Hu H.H., Chen D.Q., Wang Y.N., et al. New insights into TGF-β/Smad signaling in tissue fibrosis. Chem Biol Interact. 2018 Aug 25;292:76-83. doi: 10.1016/j.cbi.2018.07.008. Epub 2018 Jul 11. PMID: 30017632.
- Dewidar B., Meyer C., Dooley S., et al. TGF-β in Hepa–tic Stellate Cell Activation and Liver Fibrogenesis-Updated 2019. Cells. 2019 Nov 11;8(11):1419. doi: 10.3390/cells8111419. PMID: 31718044; PMCID: PMC6912224.
- Li H., Liu T., Yang Y., et al. Interplays of liver fibrosis-asso–ciated microRNAs: Molecular mechanisms and implications in diagnosis and therapy. Genes Dis. 2022 Sep 5;10(4):1457-1469. doi: 10.1016/j.gendis.2022.08.013. PMID: 37397560; PMCID: PMC10311052.
- Xu F., Liu C., Zhou D., et al. TGF-β/SMAD Pathway and Its Regulation in Hepatic Fibrosis. The Journal of Histochemistry and Cytochemistry: Official Journal of the Histochemistry Society. 2016 Mar;64(3):157-167. DOI: 10.1369/0022155415627681. PMID: 26747705; PMCID: PMC4810800.
- Roehlen N., Crouchet E., Baumert T.F. Liver Fibrosis: Mechanistic Concepts and Therapeutic Perspectives. Cells. 2020 Apr 3;9(4):875. doi: 10.3390/cells9040875. PMID: 32260126; PMCID: PMC7226751.
- Yao W., Wang T., Huang F. p300/CBP as a Key Nutritional Sensor for Hepatic Energy Homeostasis and Liver Fibrosis. Biomed Res Int. 2018 May 15;2018:8168791. doi: 10.1155/2018/8168791. PMID: 29862292; PMCID: PMC5976926.
- Morral N., Liu S., Conteh A.M., et al. Aberrant gene expression induced by a high fat diet is linked to H3K9 acetylation in the promoter-proximal region. Biochim Biophys Acta Gene Regul Mech. 2021 Mar;1864(3):194691. doi: 10.1016/j.bbagrm.2021.194691. Epub 2021 Feb 6. PMID: 33556624; PMCID: PMC7933127.
- Gates L.A., Shi J., Rohira A.D., et al. Acetylation on histone H3 lysine 9 mediates a switch from transcription initiation to elongation. J Biol Chem. 2017 Sep 1;292(35):14456-14472. doi: 10.1074/jbc.M117.802074. Epub 2017 Jul 17. PMID: 28717009; PMCID: PMC5582839.
- Etchegaray J.P., Zhong L., Li C., et al. The Histone Deacety–lase SIRT6 Restrains Transcription Elongation via Promoter-Proximal Pausing. Mol Cell. 2019 Aug 22;75(4):683-699.e7. doi: 10.1016/j.molcel.2019.06.034. Epub 2019 Aug 6. PMID: 31399344; PMCID: PMC6907403.
- Liu Y., Jiang L., Sun C., et al. Insulin/Snail1 axis ameliorates fatty liver disease by epigenetically suppressing lipogenesis. Nat Commun. 2018 Jul 16;9(1):2751. doi: 10.1038/s41467-018-05309-y. PMID: 30013137; PMCID: PMC6048127.
- Sen R., Pezoa S.A., Carpio Shull L., et al. Kat2a and Kat2b Acetyltransferase Activity Regulates Craniofacial Cartilage and Bone Differentiation in Zebrafish and Mice. J Dev Biol. 2018 Nov 12;6(4):27. doi: 10.3390/jdb6040027. PMID: 30424580; PMCID: PMC6315545.
- Xu X., Deng X., Chen Y., et al. SIRT1 mediates nutritio–nal regulation of SREBP-1c-driven hepatic PNPLA3 transcription via modulation of H3k9 acetylation. Genes Environ. 2022 May 27;44(1):18. doi: 10.1186/s41021-022-00246-1. PMID: 35624499; PMCID: PMC9137095.
- Wu T., Liu Y.H., Fu Y.C., et al. Direct evidence of sirtuin downregulation in the liver of non-alcoholic fatty liver disease patients. Ann Clin Lab Sci. 2014 Fall;44(4):410-8. PMID: 25361925.
- Nassir F., Ibdah J.A. Sirtuins and nonalcoholic fatty liver di–sease. World J Gastroenterol. 2016 Dec 14;22(46):10084-10092. doi: 10.3748/wjg.v22.i46.10084. PMID: 28028356; PMCID: PMC5155167.
- Ding R.B., Bao J., Deng C.X. Emerging roles of SIRT1 in fatty liver diseases. Int J Biol Sci. 2017 Jul 6;13(7):852-867. doi: 10.7150/ijbs.19370. PMID: 28808418; PMCID: PMC5555103.
- Singh V., Ubaid S. Role of Silent Information Regulator 1 (SIRT1) in Regulating Oxidative Stress and Inflammation. Inflammation. 2020 Oct;43(5):1589-1598. doi: 10.1007/s10753-020-01242-9. Erratum in: Inflammation. 2021 Oct;44(5):2142. PMID: 32410071.
- Zeng C., Chen M. Progress in Nonalcoholic Fatty Liver Disease: SIRT Family Regulates Mitochondrial Biogenesis. Biomole–cules. 2022 Aug 5;12(8):1079. doi: 10.3390/biom12081079. PMID: 36008973; PMCID: PMC9405760.
- Abaturov O., Nikulina A. Role of genetic modification of the PNPLA3 gene in predicting metabolically unhealthy obesity and meta–bolic associated fatty liver disease in children. Eur J Clin Exp Med. 2023;21(1):5-13. doi: 10.15584/ejcem.2023.1.1.
- Chen M., Hui S., Lang H., et al. SIRT3 Deficiency Promotes High-Fat Diet-Induced Nonalcoholic Fatty Liver Disease in Correlation with Impaired Intestinal Permeability through Gut Microbial Dysbiosis. Mol Nutr Food Res. 2019 Feb;63(4):e1800612. doi: 10.1002/mnfr.201800612. Epub 2018 Dec 27. PMID: 30525304.
- Sun R., Kang X., Zhao Y., et al. Sirtuin 3-mediated deacety–lation of acyl-CoA synthetase family member 3 by protocatechuic acid attenuates non-alcoholic fatty liver disease. Br J Pharmacol. 2020 Sep;177(18):4166-4180. doi: 10.1111/bph.15159. Epub 2020 Aug 9. PMID: 32520409; PMCID: PMC7443473.
- Nassir F. Role of acetylation in nonalcoholic fatty liver di–sease: a focus on SIRT1 and SIRT3. Explor Med. 2020;1:248-58. https://doi.org/–10.37349/emed.2020.00017.
- Martinou E., Pericleous M., Stefanova I., et al. Diagnostic Modalities of Non-Alcoholic Fatty Liver Disease: From Biochemical Biomarkers to Multi-Omics Non-Invasive Approaches. Diagnostics (Basel). 2022 Feb 4;12(2):407. doi: 10.3390/diagnostics12020407. PMID: 35204498; PMCID: PMC8871470.
- Kochumon S., Jacob T., Koshy M., et al. Palmitate Potentiates Lipopolysaccharide-Induced IL-6 Production via Coordinated Acetylation of H3K9/H3K18, p300, and RNA Polymerase II. J Immunol. 2022 Aug 15;209(4):731-741. doi: 10.4049/jimmunol.2100928. Epub 2022 Jul 27. PMID: 35896337.
- Mikula M., Majewska A., Ledwon J.K., et al. Obesity increases histone H3 lysine 9 and 18 acetylation at Tnfa and Ccl2 genes in mouse liver. Int J Mol Med. 2014 Dec;34(6):1647-54. doi: 10.3892/ijmm.2014.1958. Epub 2014 Oct 3. PMID: 25319795.
- Aseem S.O., Jalan-Sakrikar N., Chi C., et al. Epigenomic Evaluation of Cholangiocyte Transforming Growth Factor-β Signaling Identifies a Selective Role for Histone 3 Lysine 9 Acetylation in Bi–liary Fibrosis. Gastroenterology. 2021 Feb;160(3):889-905.e10. doi: 10.1053/j.gastro.2020.10.008. Epub 2020 Oct 12. PMID: 33058867; PMCID: PMC7878301.
- Zhou L., Wang L., Lu L., et al. Inhibition of miR-29 by TGF-beta-Smad3 signaling through dual mechanisms promotes transdifferentiation of mouse myoblasts into myofibroblasts. PLoS One. 2012;7(3):e33766. doi: 10.1371/journal.pone.0033766. Epub 2012 Mar 16. PMID: 22438993; PMCID: PMC3306299.
- Yamaguchi T., Yoshida K., Murata M., et al. Smad3 Phospho-Isoform Signaling in Nonalcoholic Steatohepatitis. Int J Mol Sci. 2022 Jun 3;23(11):6270. doi: 10.3390/ijms23116270. PMID: 35682957; PMCID: PMC9181097.
- Matsumoto Y., Itami S., Kuroda M., et al. MiR-29a Assists in Preventing the Activation of Human Stellate Cells and Promotes Recovery from Liver Fibrosis in Mice. Mol Ther. 2016 Oct;24(10):1848-1859. doi: 10.1038/mt.2016.127. Epub 2016 Jun 23. PMID: 27480597; PMCID: PMC5112039.
- Fu J., Wu B., Zhong S., et al. miR-29a-3p suppresses hepatic fibrosis pathogenesis by modulating hepatic stellate cell proliferation via targeting PIK3R3 gene expression. Biochem Biophys Res Commun. 2020 Sep 3;529(4):922-929. doi: 10.1016/j.bbrc.2020.06.102. Epub 2020 Jul 30. PMID: 32819600.
- Lin C.L., Lee P.H., Hsu Y.C., et al. MicroRNA-29a promotion of nephrin acetylation ameliorates hyperglycemia-induced podocyte dysfunction. J Am Soc Nephrol. 2014 Aug;25(8):1698-709. doi: 10.1681/ASN.2013050527. Epub 2014 Feb 27. PMID: 24578127; PMCID: PMC4116051.
- Smyth A., Callaghan B., Willoughby C.E., et al. The Role of miR-29 Family in TGF-β Driven Fibrosis in Glaucomatous Optic Neuropathy. Int J Mol Sci. 2022 Sep 6;23(18):10216. doi: 10.3390/ijms231810216. PMID: 36142127; PMCID: PMC9499597.
- Roderburg C., Urban G.W., Bettermann K., et al. Micro-RNA profiling reveals a role for miR-29 in human and murine liver fibrosis. Hepatology. 2011 Jan;53(1):209-18. doi: 10.1002/hep.23922. Epub 2010 Oct 1. PMID: 20890893.
- Huang Y.-H., Yang Y.-L., Wang F.-S. The Role of miR-29a in the Regulation, Function, and Signaling of Liver Fibrosis. Int. J. Mol. Sci. 2018;19:1889. https://doi.org/10.3390/ijms19071889.
- Huang Y.H., Tiao M.M., Huang L.T., et al. Activation of Mir-29a in Activated Hepatic Stellate Cells Modulates Its Profibrogenic Phenotype through Inhibition of Histone Deacetylases 4. PLoS One. 2015 Aug 25;10(8):e0136453. doi: 10.1371/journal.pone.0136453. PMID: 26305546; PMCID: PMC4549141.
- Lin H.-Y., Wang F.-S., Yang Y.-L., et al. MicroRNA-29a Suppresses CD36 to Ameliorate High Fat Diet-Induced Steatohepatitis and Liver Fibrosis in Mice. Cells. 2019;8:1298. https://doi.org/–10.3390/cells8101298.
- Liu Y., Wen D., Ho C., et al. Epigenetics as a versatile regulator of fibrosis. J Transl Med. 2023 Mar 2;21(1):164. doi: 10.1186/s12967-023-04018-5. PMID: 36864460; PMCID: PMC9983257.
- Qin L., Han Y.P. Epigenetic repression of matrix metalloproteinases in myofibroblastic hepatic stellate cells through histone deacetylases 4: implication in tissue fibrosis. Am J Pathol. 2010 Oct;177(4):1915-28. doi: 10.2353/ajpath.2010.100011. Epub 2010 Sep 16. PMID: 20847282; PMCID: PMC2947286.
- Roeb E. Matrix metalloproteinases and liver fibrosis (translational aspects). Matrix Biol. 2018 Aug;68-69:463-473. doi: 10.1016/j.matbio.2017.12.012. Epub 2017 Dec 28. PMID: 29289644.
- Roderfeld M. Matrix metalloproteinase functions in hepa–tic injury and fibrosis. Matrix Biol. 2018 Aug;68-69:452-462. doi: 10.1016/j.matbio.2017.11.011. Epub 2017 Dec 6. PMID: 29221811.
- Siersbæk M., Varticovski L., Yang S., et al. High fat diet-–induced changes of mouse hepatic transcription and enhancer activity can be reversed by subsequent weight loss. Sci Rep. 2017 Jan 10;7:40220. doi: 10.1038/srep40220. PMID: 28071704; PMCID: PMC5223143.
- Ma J., You D., Chen S, et al. Epigenetic association study uncovered H3K27 acetylation enhancers and dysregulated genes in high-fat-diet-induced nonalcoholic fatty liver disease in rats. Epigenomics. 2022 Dec;14(23):1523-1540. doi: 10.2217/epi-2022-0362. Epub 2023 Feb 22. PMID: 36851897.
- Nammo T., Udagawa H., Funahashi N., et al. Genome-wide profiling of histone H3K27 acetylation featured fatty acid signalling in pancreatic beta cells in diet-induced obesity in mice. Diabetologia. 2018 Dec;61(12):2608-2620. doi: 10.1007/s00125-018-4735-7. Epub 2018 Oct 3. PMID: 30284014.
- Becares N., Gage M.C., Voisin M., et al. Impaired LXRα Phosphorylation Attenuates Progression of Fatty Liver Disease. Cell Rep. 2019 Jan 22;26(4):984-995.e6. doi: 10.1016/j.celrep.2018.12.094. PMID: 30673619; PMCID: PMC6344342.
- Gao J., Wei B., Liu M., et al. Endothelial p300 Promotes Portal Hypertension and Hepatic Fibrosis Through C-C Motif Chemokine Ligand 2-Mediated Angiocrine Signaling. Hepatology. 2021 Jun;73(6):2468-2483. doi: 10.1002/hep.31617. Epub 2021 Apr 19. PMID: 33159815; PMCID: PMC8102654.
- Akhter N., Kochumon S., Hasan A., et al. IFN-γ and LPS Induce Synergistic Expression of CCL2 in Monocytic Cells via H3K27 Acetylation. J Inflamm Res. 2022 Jul 27;15:4291-4302. doi: 10.2147/JIR.S368352. PMID: 35923906; PMCID: PMC9343018.
- Liu X., Xu J., Rosenthal S., et al. Identification of Li–neage-Specific Transcription Factors That Prevent Activation of Hepatic Stellate Cells and Promote Fibrosis Resolution. Gastroenterology. 2020 May;158(6):1728-1744.e14. doi: 10.1053/j.gastro.2020.01.027. Epub 2020 Jan 23. PMID: 31982409; PMCID: PMC7252905.
- Garbuzenko D.V. Mechanisms of Epigenetic Regulation in the Fibrogenic Activation of Hepatic Stellate Cells in Non-alcoholic Fatty Liver Disease. Gene Expression 2024;23(1):31-43. doi: 10.14218/GE.2023.00090.
- Assante G., Chandrasekaran S., Ng S., et al. Acetyl-CoA metabolism drives epigenome change and contributes to carcinogenesis risk in fatty liver disease. Genome Med. 2022 Jun 23;14(1):67. doi: 10.1186/s13073-022-01071-5. Erratum in: Genome Med. 2023 May 18;15(1):38. PMID: 35739588; PMCID: PMC9219160.
- Guo Y., Miao X., Sun X., et al. Zinc finger transcription factor Egf1 promotes non-alcoholic fatty liver disease. JHEP Rep. 2023 Mar 9;5(6):100724. doi: 10.1016/j.jhepr.2023.100724. PMID: 37234276; PMCID: PMC10206499.
- Kong M., Chen X., Lv F., et al. Serum response factor (SRF) promotes ROS generation and hepatic stellate cell activation by epigenetically stimulating NCF1/2 transcription. Redox Biol. 2019 Sep;26:101302. doi: 10.1016/j.redox.2019.101302. Epub 2019 Aug 15. PMID: 31442911; PMCID: PMC6831835.
- de Conti A., Dreval K., Tryndyak V., et al. Inhibition of the Cell Death Pathway in Nonalcoholic Steatohepatitis (NASH)-Related Hepatocarcinogenesis Is Associated with Histone H4 lysine 16 Deacetylation. Mol Cancer Res. 2017 Sep;15(9):1163-1172. doi: 10.1158/1541-7786.MCR-17-0109. Epub 2017 May 16. PMID: 28512251.
- Pogribny I.P., Dreval K., Kindrat I., et al. Epigenetically media–ted inhibition of S-adenosylhomocysteine hydrolase and the associated dysregulation of 1-carbon metabolism in nonalcoholic steatohepatitis and hepatocellular carcinoma. FASEB J. 2018 Mar;32(3):1591-1601. doi: 10.1096/fj.201700866R. Epub 2018 Jan 3. PMID: 29127188; PMCID: PMC6137451.